Recently, a patient in Berlin (Germany) became the 7th person in the world to be declared cured of HIV after a stem cell transplant to treat leukemia. Unlike most previous cases, this patient did not receive stem cells with a mutation that completely protects against HIV. This opens up the prospect of expanding the donor pool and increasing treatment opportunities for many people.
The man, known as patient B2, was diagnosed with HIV in 2009 and acute myeloid leukemia in 2015. As part of his cancer treatment, he received a stem cell transplant from a donor who carried just one copy of the CCR5 mutation, a genetic factor that is considered the “golden key” in helping immune cells resist HIV. Previously, scientists believed that only people with two copies of the mutation – which does not produce the CCR5 receptor for the virus to enter – could be completely cured.
After the transplant, the patient continued to take antiretroviral drugs (ART) for 3 years before voluntarily stopping treatment. Since then, and for 7 years and 3 months, all tests have detected no trace of the virus in his body. He became the second person with the longest HIV-negative period among the 7 patients announced to be cured.
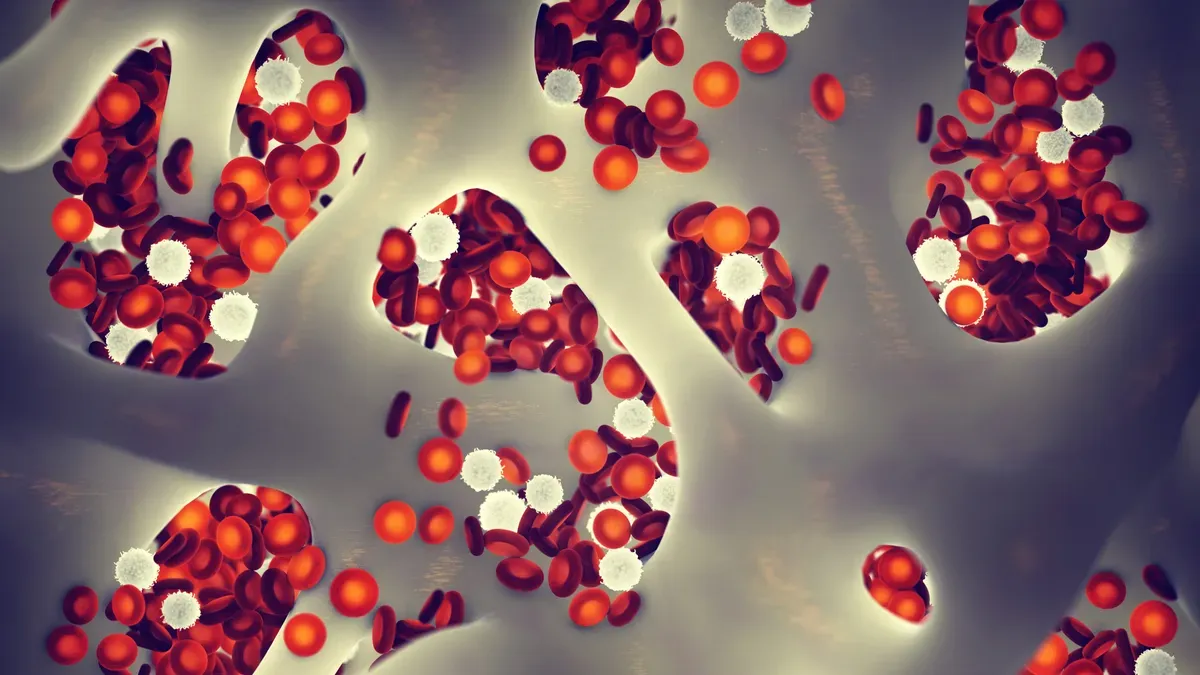
Professor Christian Gaebler, Free University of Berlin, said this result "changes the way we understand the genetic requirements for treating HIV with stem cell transplantation". According to him, the new discovery strengthens the possibility that curing HIV does not necessarily rely on stem cells carrying two CCR5 mutations as previously thought.
The mechanism of success in this case is still being studied. One theory is that the new immune cells from the donor completely eliminated the patient's old immune cells - where HIV hides - before the virus can infect the new immune system. This is a common immune response when the donor and recipient cells have certain differences in surface markers.
However, experts warn that this should not be considered a universal treatment method. Stem cell transplantation is a complex, expensive and potentially high-risk procedure, only applied when the patient also has a hematological malignancy. For the majority of people with HIV, ART remains a safe and effective option, helping to control the virus long-term. In addition, new prevention methods such as lenacapavir, which requires only two injections per year, are opening up more opportunities to protect the community.
Source: https://baolaocai.vn/nguoi-dan-ong-duoc-chua-khoi-hiv-sau-khi-ghep-te-bao-goc-post888420.html






![[Photo] Urgently help people soon have a place to live and stabilize their lives](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F09%2F1765248230297_c-jpg.webp&w=3840&q=75)








































































![[Photo] General Secretary To Lam works with the Standing Committees of the 14th Party Congress Subcommittees](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/12/09/1765265023554_image.jpeg)





























Comment (0)