Tình trạng ngộ độc thuốc tê có thể xảy ra và gây ra hậu quả nghiêm trọng đe dọa đến tính mạng bệnh nhân nếu không được xử trí kịp thời.
Ngày nay, việc sử dụng thuốc tê rất phổ biến, từ các thủ thuật thực hiện tại các cơ sở y tế bên ngoài bệnh viện như nhổ răng, tiểu phẫu vết thương… đến các thủ thuật, tiểu phẫu thuật thực hiện tại bệnh viện như: đặt catheter, chọc ống sống thắt lưng, phẫu thuật tạo hình, thẩm mỹ.
 |
| Tình trạng ngộ độc thuốc tê có thể xảy ra và gây ra hậu quả nghiêm trọng đe dọa đến tính mạng bệnh nhân nếu không được xử trí kịp thời. |
Đặc biệt, trong bối cảnh việc thực hiện kỹ thuật gây tê trước khi làm các thủ thuật này có xu hướng được thực hiện bới các bác sỹ không thuộc chuyên ngành gây mê - hồi sức, tình trạng ngộ độc thuốc tê có thể xảy ra và gây ra hậu quả nghiêm trọng đe dọa đến tính mạng bệnh nhân nếu không được xử trí kịp thời.
Mới đây, Khoa Cấp cứu, Bệnh viện Trung ương quân đội 108 tiếp nhận một bệnh nhân nam, 66 tuổi vào cấp cứu trong tình trạng xuất hiện các triệu chứng hoa mắt, chóng mặt, run chân tay sau khi nhổ răng, trong quá trình nhổ răng có sử dụng 2 ống Lidocain 2% tê tại chỗ; các dấu hiệu sinh tồn và các chỉ số xét nghiệm cơ bản đều trong giới hạn bình thường.
Bệnh nhân được chẩn đoán theo dõi ngộ độc thuốc tê Lidocain sau nhổ răng. Ngay lập tức bệnh nhân được truyền tĩnh mạch nhũ tương lipid 20%, theo dõi sát tình trạng ý thức và huyết động.
Sau khi dùng thuốc 15 phút, các triệu chứng lâm sàng khiến bệnh nhân khó chịu hết hoàn toàn. Bệnh nhân được chuyển lên Khoa Dị ứng, Bệnh viện Trung ương quân đội 108 tiếp tục theo dõi và điều trị.
Trường hợp kể trên, bệnh nhân may mắn được cấp cứu đúng cách và kịp thời nên tránh được những hậu quả đáng tiếc. Tuy nhiên, tình trạng ngộ độc thuốc tê luôn tiềm ẩn nhiều nguy hiểm (ngộ độc thuốc tê, phản vệ với thuốc tê, hội chứng sợ hãi).
Việc chẩn đoán phân biệt các giả thuyết trên thường dựa vào các triệu chứng đi kèm như bệnh nhân hoảng sợ, lo lắng quá mức trước khi làm thủ thuật (hội chứng sợ hãi); bệnh nhân khó thở, thở rít, nổi ban mề đay, ngứa, buồn nôn, đau bụng (phản vệ với thuốc); còn lại là tình trạng ngộ độc.
Trong 3 giả thuyết trên thì ngộ độc lại hay xảy ra nhất, trong khi đó phản vệ lại hiếm gặp nhất. Vì vậy, khi gặp phải tình huống lâm sàng như trên, chúng ta nên xử trí theo hướng ngộ độc thuốc kết hợp với các biện pháp hồi sức cấp cứu cơ bản thì khả năng cao sẽ cứu sống được bệnh nhân.
Ngộ độc thuốc tê nếu không được cấp cứu kịp thời sẽ để lại những hậu quả nghiêm trọng, thậm chí tử vong. Vì vậy, việc hiểu biết về những dấu hiệu nhận biết sớm và những biện pháp cấp cứu kịp thời bệnh nhân ngộ độc thuốc tê là rất quan trọng, giúp giảm nguy cơ mắc bệnh và tử vong.
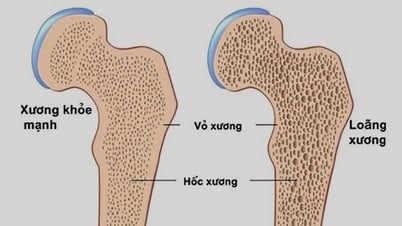
Để phòng ngừa ngộ độc thuốc tê, theo các bác sỹ của Khoa Cấp cứu, Bệnh viện Trung ương quân đội 10 cho biết, những đối tượng có nguy cơ cao ngộ độc thuốc tê là trẻ em dưới 6 tháng tuổi; bệnh nhân thể trạng nhỏ; tuổi cao, suy yếu; suy tim, thiếu máu cơ tim; bệnh gan.
Hội Gây tê vùng và Giảm đau Hoa Kỳ khuyến cáo, những thay đổi về thần kinh hoặc tim mạch của bệnh nhân khi đang sử dụng thuốc tê, dù liều nhỏ, gây tê theo phương pháp gì, cần nghĩ tới ngộ độc thuốc tê trước và xử trí theo phác đồ.
Hệ thần kinh trung ương như kích thích (bồn chồn, lo lắng, kêu la, giật cơ, co giật); ức chế (ngủ gà, hôn mê hoặc ngừng thở); triệu trứng không đặc hiệu (miệng có vị kim loại, tê quanh miệng, nhìn đôi, ù tai, chóng mặt). Với hệ tim mạch: Giai đoạn đầu có thể có bị tăng huyết áp, mạch nhanh, loạn nhịp thất…
Giai đoạn sau: Bệnh nhân có thể tụt huyết áp tiến triển; block dẫn truyền, nhịp tim chậm, vô tâm thu; loạn nhịp thất (nhanh thất, rung thất, xoắn đỉnh, vô tâm thu).
Các triệu chứng ngộ độc trên lâm sàng có thể xuất hiện chậm sau 30 phút hoặc muộn hơn. Cần giao tiếp thường xuyên với bệnh nhân để phát hiện sớm các dấu hiệu ngộ độc.
Người bệnh cần nắm rõ các dấu hiệu nhận biết sớm tình trạng ngộ độc thuốc tê để khi xảy ra có thể đến các cơ sở y tế gần nhất cấp cứu kịp thời.
Và tại các cơ sở y tế cũng cần luôn luôn có bộ cấp cứu ngộ độc thuốc tê cũng giống như bộ cấp cứu phản vệ. Nhũ tương lipid là thuốc đầu tay ngay khi có biểu hiện đầu tiên và rõ ràng của ngộ độc thuốc tê do bất kỳ loại thuốc tê nào và liều adrenaline ≤ 1mcg/kg là hiệu quả hơn trong hồi sinh tim phổi nâng cao ở bệnh nhân ngừng tim hoặc tụt huyết áp do ngộ độc thuốc tê.
Nguồn: https://baodautu.vn/nguy-co-tiem-an-khi-su-dung-thuoc-gay-te-d221034.html






![[Ảnh] Thủ tướng Phạm Minh Chính tiếp lãnh đạo một số tập đoàn hàng đầu Brazil](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/7/6/3622160b379746e6bca82f804ea35e47)












































































![[REVIEW OCOP] Bánh gai Bảy Quyên: Đặc sản quê vươn tầm nhờ uy tín thương hiệu](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/7/3/1a7e35c028bf46199ee1ec6b3ba0069e)










Bình luận (0)