In Hanoi , Anh Hung, 31 years old, had been experiencing difficulty swallowing and vomiting after eating for the past month. He initially thought it was acid reflux, but doctors discovered he had acute gastritis with achalasia.
Mr. Thai Huu Hung (from Bac Ninh ) came to Tam Anh General Hospital in Hanoi for examination because his symptoms were worsening, he had lost 12 kg (from 71 kg to 59 kg), and was malnourished. Previously, he had consulted many doctors and been diagnosed with gastroesophageal reflux disease, gastritis, and anxiety disorder, but the medication did not help.
This time, the gastroscopy results showed that the patient's esophagus was constricted at the junction between the esophagus and the stomach. The doctor measured esophageal motility and diagnosed the patient with type II achalasia accompanied by acute gastritis. Achalasia is a functional disorder that prevents the esophagus from pushing food down into the stomach; the lower esophageal sphincter constricts, causing food to remain in the esophagus or to reflux after eating or drinking.
On November 14th, Dr. Vu Truong Khanh, Head of the Gastroenterology Department at Tam Anh General Hospital in Hanoi, stated that the patient's symptoms are easily confused with gastroesophageal reflux disease (GERD). However, in patients with achalasia, the refluxed fluid has not yet reached the stomach, so it usually does not have a sour taste. The fluid of patients with GERD typically contains acid and has a sour taste.
The patient received intravenous nutrition and underwent endoscopic intervention using balloon esophageal dilation. One day after the procedure, the symptoms of difficulty swallowing and chest pain decreased. Mr. Hung was able to eat and drink easily, was discharged after two days, and will have regular follow-up appointments to assess his swallowing and esophageal function.

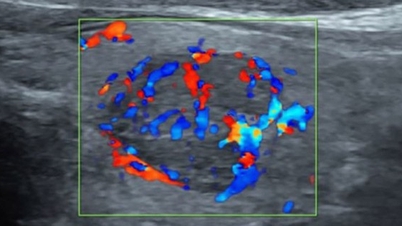
The patient recovered after esophageal dilation using a balloon. Photo: Tam Anh General Hospital.
Esophageal dilation with balloon involves using an air balloon to dilate and tear the lower esophageal sphincter muscle fibers, helping to empty the esophagus after swallowing food. This method has a long-lasting effect and is suitable for patients with type I and II achalasia, especially young patients with a short duration of the disease and without significant esophageal axial deformation. Doctors usually perform endoscopic esophageal sphincterotomy through the mouth when the disease progresses to type III.
After balloon angioplasty, patients should eat soft foods, chew thoroughly, and avoid stimulants.
Dr. Khanh stated that achalasia is usually benign, progresses slowly, but affects health and quality of life. Symptoms are easily confused with other gastrointestinal diseases.
Diagnostic methods such as gastroscopy and esophageal X-ray may miss lesions in the early stages. If left untreated, the disease can lead to many complications such as esophagitis, malnutrition, pneumonia, and cancer in areas of chronic inflammation.
People experiencing symptoms of reflux and vomiting that do not improve with treatment should seek medical attention at a gastroenterology specialist.
Emerald
| Readers can ask questions about digestive diseases here for doctors to answer. |
Source link















































































































Comment (0)