Ngoc Minh, 22, from Hanoi , suffered from shortness of breath, pleural effusion, and blood in her pleural cavity for six months, requiring continuous drainage. Doctors discovered a lymphatic malformation in her bone, a rare condition with only 39 cases recorded in world medical literature.
Previously, the patient visited four hospitals, having approximately 1-2 liters of fluid aspirated each week for about six months, and underwent numerous tests, but the cause of the hemothorax remained undetected.
On October 30th, Associate Professor Dr. Nguyen Xuan Hien, Director of the Center for Diagnostic Imaging and Interventional Radiology at Tam Anh General Hospital in Hanoi, stated that the patient was admitted with lung, bone, liver, and spleen damage; anemia, emaciation, pale skin, shortness of breath, and chest tightness. The patient's left pleural cavity was distended with fluid; doctors aspirated three liters of pinkish fluid, while the normal pleural fluid volume is 7-10 ml.
"If we continue draining the fluid, the patient will become debilitated, but if we stop, it will cause lung collapse and respiratory failure," Associate Professor Hien said.
Test results showed that the pleural fluid contained a high concentration of lipids, a substance found in lymphatic fluid. The entire thoracic duct was dilated and tortuous. The doctor concluded that the patient had a multi-organ lymphatic malformation affecting bones, liver, and spleen. The lymphatic malformation in the chest ruptured, causing fluid and blood to leak into the left pleural cavity, resulting in significant blood and nutrient loss.

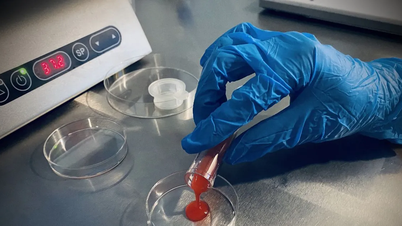
Pleural fluid after drainage from the patient. Photo: Provided by the hospital .
"Lymphangioma is rare, and lymphangioma invading bone is even rarer," Associate Professor Hien said, adding that the 2022 Chinese study published in the US National Library of Medicine is the only retrospective study to date that included 39 patients with vascular malformations invading bone; the rest are just scattered reports of a few cases. The disease is very rare and there are no specific comprehensive statistics. Therefore, it rarely receives attention, and doctors easily overlook or misdiagnose it.
The team used a thoracic duct embolization system to seal the leak. The Artis Pheno robotic system scanned the entire lymphatic system, detecting the leak at the level of the left pulmonary hilum. Associate Professor Hien sealed the leak using metal coils and biological glue. The doctor assessed this as a difficult technique because it involved directly puncturing through the epigastric region, where the lymphatic ducts were extremely small, with a diameter of about 1.5-2 mm, making them difficult to locate and seal, requiring highly experienced surgeons.

Doctors embolize the lymphatic fistula on the patient. Photo: Provided by the hospital .
After an hour of intervention, the doctor successfully sealed the leak. After one day, the pleural effusion decreased significantly, to 10% of what it was before the intervention. The patient could breathe easily, eat well, and the pleural effusion cleared after 5 days, allowing for discharge from the hospital.
Common lymphatic malformations are usually harmless and almost asymptomatic, making them difficult to detect. Most cases are discovered during trauma or surgery when the tumor ruptures, causing fluid to leak into the pleural, peritoneal, or pericardial cavities. In some cases, an enlarged liver, enlarged spleen, or spontaneous bone fracture may be discovered incidentally.
According to Associate Professor Hien, typically, when a lymphatic vessel ruptures, doctors use MRI to locate the leak, but this method is time-consuming and expensive. Currently, Tam Anh General Hospital in Hanoi uses computed tomography (CT) scans of the lymphatic system, which helps to accurately detect the location of the lymphatic fistula. This diagnostic technique is faster and cheaper than MRI.
Lymphatic vascular tumors are an incurable disease as there is no specific cure. One of the complications of the disease is lymphatic fistula, at which point the patient should undergo radiological intervention. With the help of advanced equipment, doctors can accurately locate and block the fistula point, causing no pain or blood loss, and allowing for a quick recovery.
Hoai Pham
| Readers can post questions about respiratory illnesses here for doctors to answer. |
Source link















































































































Comment (0)