Medical news October 2: Severe malnutrition in children due to congenital heart disease
Congenital heart disease in children will cause many health consequences if not treated promptly.
Severe malnutrition due to congenital heart disease
Tam Anh General Hospital in Ho Chi Minh City has just admitted a 3-month-old baby weighing only 3.6 kg (3.1 kg at birth), with difficulty breathing due to pulmonary hypertension and severe heart failure.
The baby's mother said that the baby breastfed intermittently, had difficulty breathing, sweated a lot while breastfeeding, and was slow to gain weight. An echocardiogram determined that the baby had a large ventricular septal defect (8 mm) leading to heart failure.
A ventricular septal defect occurs when one or more holes appear in the wall between the left ventricle and the right ventricle.
At that time, oxygen-rich blood from the left ventricle flows into the right ventricle and then straight to the pulmonary artery, increasing the volume and pressure in the pulmonary circulatory system as well as increasing the amount of blood returning to the left heart. At the same time, the heart has to work harder, gradually causing the heart to dilate.
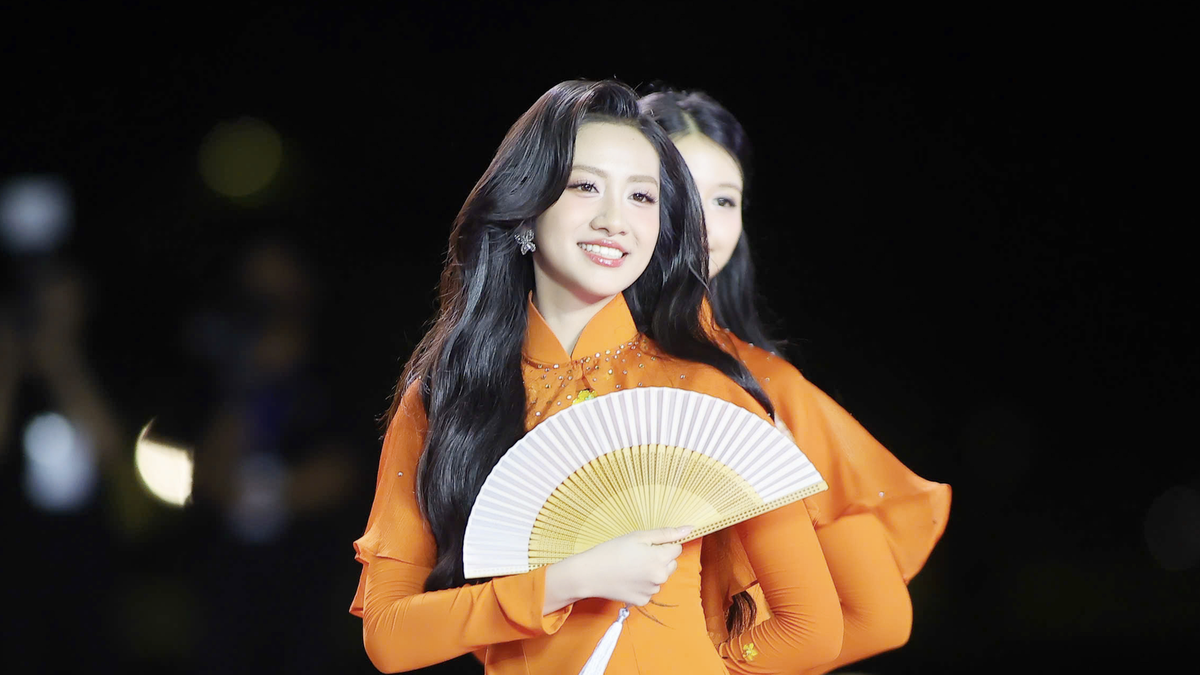
 |
| Illustration |
According to Dr. Nguyen Minh Tri Vien, Cardiac Surgery Consultant, Cardiovascular Center, Tam Anh General Hospital, Ho Chi Minh City, the child is always in a state of difficulty breathing, poor appetite, slow weight gain, and needs early intervention to close the ventricular septal defect to improve breathing and help the child develop healthily.
If treatment is delayed, complications can easily occur such as dilated heart chambers, increased pulmonary artery pressure causing damage to the pulmonary artery, endocarditis (infection on the inner surface of the heart), and severe malnutrition due to poor eating and absorption.
Doctors are concerned because the patient is malnourished, has heart failure, and severe pulmonary hypertension. These are factors that make the anesthesia and resuscitation process very difficult.
During anesthesia, care must be taken not to expose the baby to painful stimulation as this will aggravate pulmonary hypertension.
After the baby is in a deep sleep, the doctor will perform endotracheal intubation and continue to perform erector spinae plane (ESP) anesthesia to help reduce pain during surgery by up to 90%, limiting the need for morphine after surgery.
Because the baby's body is too thin, it is difficult to determine the muscle layer during the procedure. We must rely on the support of a high-resolution ultrasound system to locate the erector spinae muscle plane, thereby accurately threading the guidewire.
In addition, the concentration of anesthetic must also be suitable for a malnourished baby. If overdosed, it can easily cause anesthetic poisoning or damage to the nervous system.
The anesthesia process was completed. Doctor Vien and his team began the surgery, using autologous tissue (to avoid rejection after surgery) to patch the hole in the septum between the two ventricles. The surgery ended successfully after 3 hours.
The patient was extubated early, only 4 hours after surgery, gradually reduced medications, and discharged 5 days later.
A week after discharge, the baby's mother reported that the baby was breastfeeding better, no longer sweating while breastfeeding, sleeping well at night, the surgical wound had healed, and the baby had gained 4.2 kg in weight. The baby continued to be monitored and re-examined periodically according to the appointment schedule.
Dr. Thuy said that ventricular septal defect is the most common congenital heart disease, accounting for more than 37% of all congenital heart diseases in children, with an incidence of about 0.3% in newborns.
Small ventricular septal defects (less than 3 mm) usually do not require treatment because the defect will close on its own as the child grows. For medium-sized ventricular septal defects (3-under 5 mm in diameter) and large ventricular septal defects (5 mm or more in diameter), the possibility of spontaneous closure is very low. At this time, treatment methods for closing the defect include percutaneous closure of the defect and open-heart surgery to patch the defect.
Signs of medium-sized to large ventricular septal defects may appear within the first month after birth. Small defects often do not show symptoms until adulthood.
Therefore, it is very necessary for pregnant women to go for check-ups, have ultrasounds on schedule, and have congenital heart disease screening after the baby is born until it grows up, to help detect the disease early, have a suitable monitoring and treatment plan, Dr. Thuy recommends.
In Vietnam, on average, more than 1.5 million children are born each year, of which about 10,000-12,000 children have congenital heart disease.
Worldwide , each year about 1-1.5 million children are born with congenital malformations. About 1/4 of children with heart defects need surgery within the first year of life, and 4.2% of newborn deaths are due to congenital heart defects.
Warning about the habit of self-treating at home with leaves and herbal medicine
Vietnam - Sweden Uong Bi Hospital ( Quang Ninh ) has just received and treated 2 patients with complications and skin infections due to self-treatment at home with herbal medicine and leaves for burns and psoriasis.
The patient (2 years old, residing in Dong Trieu, Quang Ninh) was burned by boiling water at home. After receiving first aid at a medical center near his home, instead of being transferred to a higher level for complete treatment, the family asked to go home and apply traditional medicine themselves in the hope that the wound would heal quickly.
As a result, after only 2 days of applying herbal medicine, the patient's burns on the buttocks, genitals, legs, and feet became red and oozed fluid. At this time, the family took the child to the Vietnam - Sweden Uong Bi Hospital for emergency treatment.
The second patient had psoriasis but did not follow the doctor's treatment regimen and instead bathed with some leaves as many people advised.
After a few baths, the patient saw many skin burns appear, accompanied by a feeling of heat, burning, and pain at the burns.
Doctors at the Vietnam-Sweden Uong Bi Hospital said that despite repeated warnings, there are still many cases of hospitalization with complications such as ulcers, infections, necrosis, etc. caused by improper self-treatment. Therefore, each person should protect their own health by visiting and listening to the doctor's advice when there are unusual health problems.
In fact, there are many cases where patients have self-treated at home using word-of-mouth remedies and folk remedies.
These treatments have not been scientifically proven and the result is that the disease does not improve but tends to get worse. Then the patient rushes to the hospital, making treatment difficult, prolonging the treatment time and causing a lot of pain for the patient.
Stress Eliminates Liver Tumors
Doctors at the Central Hospital for Tropical Diseases have just undergone 9 hours of intense surgery to remove a malignant liver tumor that had progressed to the final stage, invading the inferior vena cava and portal vein of a 42-year-old male patient.
Male patient D.NT was admitted to the Department of Hepatobiliary, Digestive and Oncology Surgery, Central Hospital for Tropical Diseases with a large liver tumor of nearly 20cm invading the diaphragm, with thrombosis of the common portal vein and inferior vena cava spreading close to the heart.
The tumor is very large, often causing pain to the patient, with the risk of rupture at any time. In addition, portal vein thrombosis can also lead to acute liver failure and complications such as ruptured esophageal varices. In particular, inferior vena cava thrombosis has a high risk of death.
Based on the medical history, patient T. was diagnosed with active hepatitis B in 2014. However, due to his busy life, the patient did not comply with treatment. In early 2024, the patient began to feel pain in the right hypochondrium and severe weight loss, about 8-10kg. In May 2024, the patient was diagnosed with late-stage liver cancer.
Specialist II Doctor Nguyen Truong Giang, Department of Hepatobiliary, Digestive and Oncology Surgery, said that the patient's tumor not only caused constant pain but also had the risk of rupturing at any time. If not operated on, it would lead to acute liver failure, causing rapid death.
When admitting the patient, the doctors considered three main factors in this case. First, the patient was only 42 years old, and his basic body functions were still stable. The patient was able to endure a major surgery. Regarding liver function, before surgery, the patient's liver function tests showed that the remaining liver after the right hepatectomy was still enough to maintain function, minimizing the risk of postoperative liver failure.
Although the patient has advanced cancer, the goal of surgery is not to cure the disease but to prolong life and improve quality of life.
Dr. Giang said that this was a very difficult surgery, because the patient was in an extremely late stage, with a large tumor invading the main blood vessels. The success rate in cases like this is very low. But surgery is the only option at the moment.
The surgery lasted nearly 9 hours, including complete removal of the right liver (nearly 20cm in size), removal of a thrombus from the inferior vena cava and reconstruction of the blood vessels.
During surgery, patients must use an extracorporeal circulatory support system to maintain stable blood circulation. In particular, doctors face great challenges with coagulation disorders, massive blood loss, and severe metabolic acidosis.
After surgery, the patient was transferred to the Intensive Care Unit, and his condition began to improve after two days. On the fifth day after surgery, the patient's breathing tube was removed and his organs gradually recovered. The patient is now stable and has been discharged from the hospital.
Dr. Giang added that at this time, there is no optimal treatment regimen in the world for advanced liver cancer cases like the patient's.
Surgery remains the treatment option with the highest success rate. However, medical staff must monitor the recovery process extremely closely to avoid dangerous complications.






























































































Comment (0)