The patient was previously healthy and went to the doctor because of suspected food poisoning. At Bach Mai Hospital, the doctor ordered a CT scan of the abdomen and a colonoscopy. The results showed a large ulcerated mass in the colon, occupying the entire circumference of the colon, and the endoscope could not pass through, so a biopsy was ordered.
On May 6, Dr. Pham Cam Phuong, Director of the Center for Nuclear Medicine and Oncology, Bach Mai Hospital, said the biopsy results confirmed stage 3 colon cancer with lymph node metastasis.
The patient is indicated for hospitalization for further diagnosis and appropriate treatment regimen.
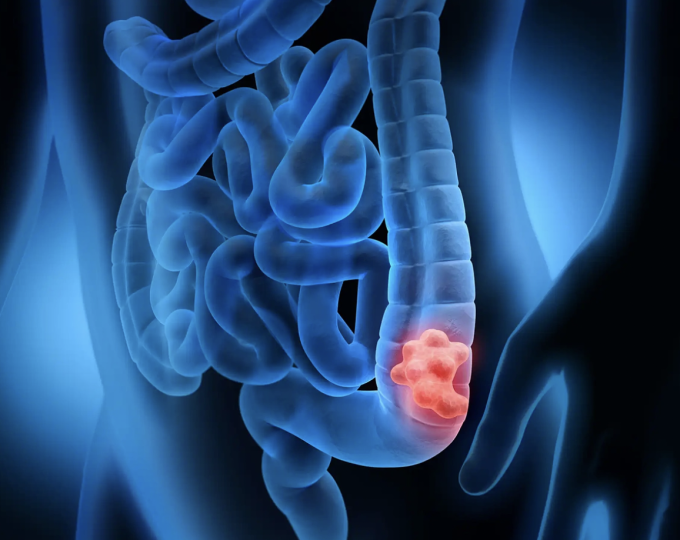
Illustration of colon cancer tumor.
According to statistics from the World Cancer Organization (Globocan) in 2020, Vietnam had more than 14,000 new cases and more than 7,500 deaths from colorectal cancer. Worryingly, the disease is on the rise in the 30-40 age group, even under 20 years old. The incidence of colon cancer is increasing over time, especially in urban areas due to changes in lifestyle and diet.
Risk factors for colon cancer include a family history of colon cancer; colon polyps, chronic bowel inflammation (such as ulcerative colitis, Crohn's) or an unhealthy diet and lifestyle.
People can reduce the risk of cancer by making small changes in their daily lives. Eat more vegetables, fruits, whole grains, limit red meat, processed meat. Increase physical activity and maintain exercise at least 30 minutes/day, limit stimulants, get enough sleep every day.
According to the American Cancer Society, people from 45 years old should be screened even if they have no symptoms. For people with high risk factors (personal history of colorectal cancer or colorectal polyps, family history of colorectal cancer, inflammatory bowel disease, history of abdominal or pelvic radiation therapy), screening should be done earlier, even from 20-30 years old.
Kim Ly (According to Vnexpress.net)
Source: http://baovinhphuc.com.vn/Multimedia/Images/Id/127975/Tuong-ngo-doc-thuc-an-hoa-ung-thu



























































































Comment (0)