If brain tumors are not operated on promptly, the risk of death or sequelae such as hemiplegia and loss of language ability is very high.
Medical news on December 26: AI Robot application to perform brain tumor surgery to save patient
If brain tumors are not operated on promptly, the risk of death or sequelae such as hemiplegia and loss of language ability is very high.
AI Robot Surgery Saves the Life of a Patient with Dangerous Brain Hemangioma
A 26-year-old male patient named Tu went to the hospital for a check-up when he discovered abnormalities in his health. The 3 Tesla MRI scan results showed that Tu had a cavernous hemangioma in the left thalamus, measuring 3x3 cm, with bleeding inside the tumor.
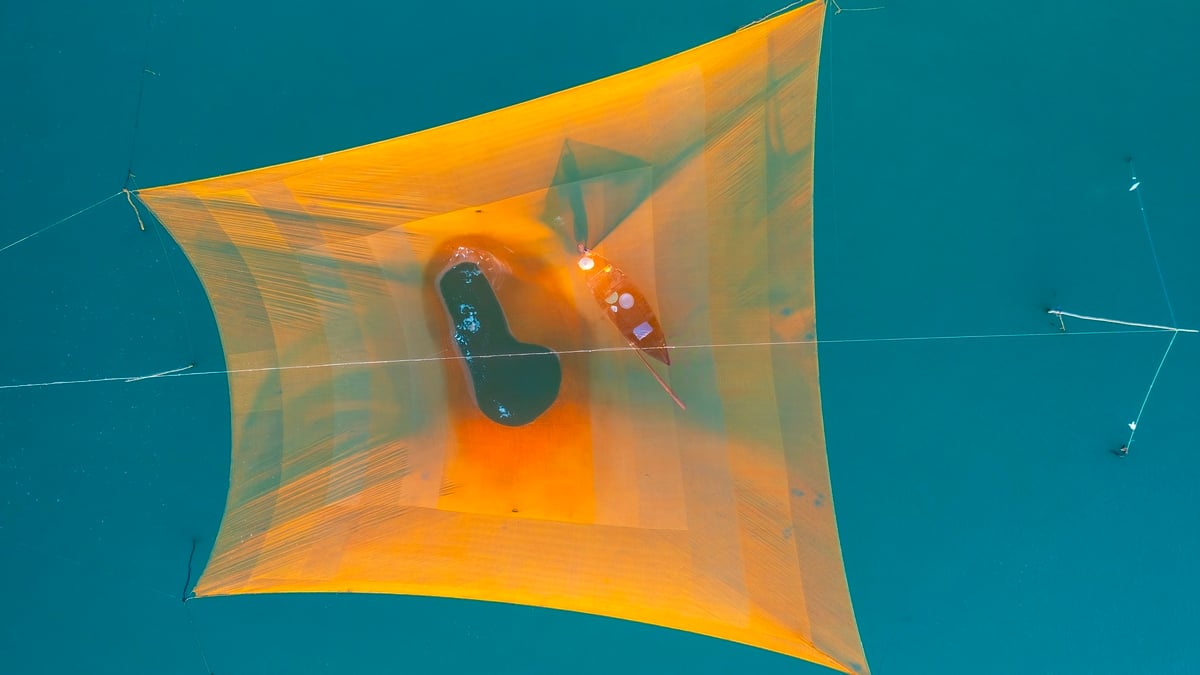
 |
| Brain tumor image of patient. |
This is a very dangerous location, the thalamus is located deep in the brain and plays a central role in transmitting nerve impulses. Damage to this area can cause death or leave severe neurological sequelae.
MSc. Dr. Mai Hoang Vu, Department of Neurosurgery, Tam Anh General Hospital, Ho Chi Minh City, said that bleeding in the tumor causes the tumor to increase in size rapidly, with the risk of sudden rupture leading to deep bleeding in the left brain and hemorrhagic stroke.
Without timely surgery, the risk of death or sequelae such as hemiplegia and loss of language ability is very high. Mr. Tu has had symptoms of numbness and weakness in the right side of his body for the past 6 months, but due to the high level of risk, he has not been able to undergo surgery at other medical facilities.
After receiving medical treatment and his symptoms continued to worsen, his family went to Tam Anh General Hospital in Ho Chi Minh City. After a thorough consultation, the doctors decided to perform surgery to remove the tumor for Mr. Tu using the Modus V Synaptive artificial intelligence (AI) brain and spinal cord surgery robot, which helps ensure safety during surgery and maximize protection of neurological function.
Thanks to the robot's ability to harmonize MRI, DTI, CT, DSA... images, doctors can clearly observe the location and structure of the tumor, as well as the relationship of the tumor to nerve fiber bundles and healthy brain structures. This helps doctors proactively choose the optimal surgical path and minimize risks for the patient.
Before the actual surgery, the doctors used the AI robot's simulated surgery feature to plan the surgery in detail, predicting possible situations and risks. From there, the doctors could proactively make adjustments throughout the surgery.
The surgery was performed as planned. The doctor made an incision in the left temple area, opened a 5cm incision, and approached the tumor along the path of the nerve fibers.
After 3 hours, the surgery was successful, the tumor was completely removed without causing brain blood vessel rupture. The use of AI robots helps to preserve maximum nerve fibers and healthy brain structures.
Two days after the surgery, Mr. Tu recovered well, his difficulty speaking symptoms were gone and there were no complications. However, his right-sided muscle strength improved slowly, and the doctor recommended that he continue physical therapy for the next 6-12 months. Mr. Tu is expected to be discharged in the next few days and return for a check-up a week later.
Doctor Vu said that Mr. Tu had a congenital, benign cavernous hemangioma, and the surgery completely removed the tumor, including the capsule, helping to avoid the risk of recurrence.
In Vietnam, we do not have official data on brain tumor diagnosis and the rate of patients with brain tumors each year. Viet Duc Friendship Hospital alone examines and treats more than 2,500 brain tumor patients each year.
Brain tumors are treatable. Many types of brain tumors are treated early, promptly, and properly, and patients can live, work, and function normally.
There are three main methods of treating brain tumors: surgery, radiotherapy and chemotherapy. Depending on each specific case, the doctor will decide which treatment method is most effective, or sometimes it is necessary to combine several methods together.
Brain tumors in children are different from those in adults. Children generally have longer survival times and 69% of children will survive after brain tumor treatment.
The doctor will consider the side effects of the treatment before deciding. Treatments with the fewest side effects will be preferred.
“How long will the patient live?” is a question that patients and their families with brain tumors often ask their doctors.
Answering this question, Associate Professor, Dr. Dong Van He, Deputy Director of Viet Duc Friendship Hospital, Director of the Neurosurgery Center said that the answer is not the same for everyone.
Some brain tumor patients can live a normal healthy life and their life expectancy is not significantly reduced after brain tumor treatment. Others can live for a few more months or years. Some brain tumors grow very quickly, the tumor grows rapidly after a few weeks or months. Some other cases grow very slowly, increasing by 2 - 3 mm each year.
Brain tumors can recur after treatment, but there are also types that do not recur or do not grow larger after many years. Therefore, we must be examined, consulted and monitored for brain tumors continuously and regularly.
Survival time after brain tumor treatment depends on many factors such as: tumor type, patient age, location, size, treatment method...
In the United States, about 20% of patients with malignant brain tumors survive more than 5 years after treatment. In children, the 5-year survival rate for malignant brain tumors is as high as 72%.
Children under 3 years of age have shorter survival times after treatment than children aged 3-16 years. Among brain tumors, glioblastoma multiforme has the shortest survival times after surgery.
For meningioma, the patient can be completely cured if the tumor is benign, surgery is performed early and completely removed. The patient can live a normal life.
Confusion between gastritis and myocardial infarction
Mr. Liem, 57, had been dealing with severe chest pain for seven days without realizing he was having an acute myocardial infarction. Initially, he only felt a burning sensation behind his sternum, accompanied by reflux, heartburn, and shortness of breath.
Based on these symptoms, the doctor at the local hospital diagnosed him with acid reflux and prescribed medication. However, his condition did not improve and he continued to have persistent symptoms.
A few days later, when he went to the clinic to have his stomach checked, Mr. Liem had an electrocardiogram (ECG) and discovered dangerous signs of an acute myocardial infarction.
Dr. Phan Thi Hoang Yen, a cardiologist, said his electrocardiogram showed ST elevation, a clear sign of a heart attack.
Blood tests showed his troponin level was 3,048 ng/L, while the normal level is just under 14 ng/L, indicating severe heart muscle damage. An echocardiogram also showed severe left ventricular dysfunction, with the apex of the heart no longer contracting.
Although he did not have typical symptoms such as severe chest pain or cold sweats, Mr. Liem mistook the symptoms for digestive problems. This shows the connection between the heart and the digestive system, as both are controlled by the vagus nerve, making the pain of a heart attack easily confused with stomach pain.
After discovering the critical condition, doctors here quickly implemented emergency measures, closely monitored the patient's condition and prepared for coronary intervention.
Master, Doctor, CKII Vo Anh Minh, Deputy Head of the Interventional Cardiology Department, said that Mr. Liem's heart function had decreased by more than half compared to normal. Coronary angiography results showed that the left coronary artery was severely blocked.
Mr. Liem was prescribed an emergency stent to re-open the coronary artery and restore blood flow to the heart muscle. Thanks to the timely intervention, Mr. Liem's heart failure condition improved rapidly. After 2 days, he was able to walk lightly and eat normally, and was discharged with instructions to use heart rehabilitation and anticoagulants to prevent restenosis.
Dr. Minh emphasized that many heart attack patients do not recognize their symptoms, leading to late hospitalization.
According to the European and American Society of Cardiology, the “golden time” for revascularization in the treatment of myocardial infarction is less than 60 minutes. However, the later the hospital admission, the higher the risk of death.
Doctors recommend that when experiencing unusual symptoms such as chest pain, shortness of breath, abdominal pain, bloating, dizziness, or neck pain, patients should go to a reputable medical facility for examination, electrocardiogram, and blood tests to detect early and avoid serious risks.
Detect osteomyelitis from heel pain symptoms
Patient NTC, 67 years old, from Ba Vi, Hanoi , had been suffering from pain in her right heel for 5 months. Initially, she bought painkillers and anti-inflammatory drugs to treat at home, but only saw slight improvement and did not completely cure it. Then, she decided to go to Medlatec General Hospital for examination and discovered that she had osteomyelitis - a serious bone infection.
Upon admission to the hospital, Ms. C. told the doctor that the pain in her right heel increased when walking and had lasted for 5 months. She had previously had an ankle X-ray taken at a local medical facility and discovered a heel spur, which she then self-treated but to no avail.
At Medlatec, Dr. Trinh Thi Nga ordered an X-ray and ultrasound of the heel, which detected a bone defect and a subperiosteal abscess. Suspecting osteomyelitis, the doctor ordered an additional magnetic resonance imaging (MRI), which showed bone marrow edema, continuous loss of the calcaneal tuberosity, and widespread damage to the surrounding soft tissues. The doctor diagnosed the patient with osteomyelitis of the right heel.
Osteomyelitis is a bone infection caused by bacteria or viruses that enter the bone through three main routes: blood, direct infection (after surgery or trauma), or from nearby structures (arthritis, soft tissue inflammation).
In Ms. C.’s case, although she had no history of trauma or surgery to her heel, due to her agricultural work and frequent exposure to mud, she may have been infected with bacteria through small scratches on her feet. Over time, the bacteria penetrated deeper and caused osteomyelitis.
Osteomyelitis can progress through three stages: acute, subacute, and chronic. The acute stage usually has symptoms such as severe pain, swelling, high fever, and reduced mobility. Meanwhile, the subacute and chronic stages have milder symptoms, but if not treated promptly, can lead to serious complications such as septic arthritis, sepsis, abscesses, pathological fractures, or bone deformities.
After diagnosis, the Russian doctor prescribed surgery to remove the infection and use antibiotics. However, due to health insurance issues, Ms. C. requested to be transferred to another hospital for further treatment.
Russian doctors recommend that when experiencing symptoms of prolonged bone pain, especially heel pain accompanied by fever, swelling or reduced mobility, patients should go to reputable medical facilities for timely examination and treatment.
Osteomyelitis can result from small but unnoticed injuries, especially in people exposed to dirty soil or contaminated environments.
Osteomyelitis can occur at any age, but is more common in children and is mainly caused by Staphylococcus aureus. In addition, some other bacteria such as streptococcus, Pseudomonas aeruginosa and fungi can also be the cause. Patients with risk factors such as a history of trauma, exposure to dirty environments, or symptoms of prolonged bone pain should be screened for osteomyelitis.
If treated promptly, osteomyelitis can be controlled, helping patients recover quickly and avoid dangerous complications. Therefore, early detection and proper treatment are very important to protect each person's health.
Source: https://baodautu.vn/tin-moi-y-te-ngay-2612-ung-dung-robot-ai-mo-u-nao-cuu-benh-nhan-d235610.html























![[Photo] Discover the "wonder" under the sea of Gia Lai](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/8/6/befd4a58bb1245419e86ebe353525f97)





![[Photo] Nghe An: Provincial Road 543D seriously eroded due to floods](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/8/5/5759d3837c26428799f6d929fa274493)























































Comment (0)