
Another successful liver transplant with incompatible blood types
In March 2023, H. discovered a liver tumor, a ruptured tumor complication, and underwent surgery in the province. After that, patient H. was transferred to the National Children's Hospital for examination and treatment, and underwent embolization twice.
In April 2025, the patient underwent the third embolization intervention at the 108 Military Central Hospital. However, the liver tumors continued to grow and increase in size. Therefore, the patient was indicated for a liver transplant.
H.'s mother, Th., looked at her daughter with heartache: "Your parents gave birth to you and raised you until now, they just want to cure your illness so you can have more health. You are still young, you have a whole future ahead of you." Even though her daughter was worried and didn't want to, her decision to donate her liver to her child was very quick.
The special point of the case of mother and child Th. is that the liver transplant was not blood type compatible (child blood type O, mother blood type B). For ABO incompatible liver transplantation, the most important issue is to reduce the amount of antibodies against antigen A and/or B in the recipient's serum to a safe level so as not to cause excessive humoral immune responses against the transplanted liver.

Master, Specialist Doctor I Nguyen Hoang Ngoc Anh, Department of Hepato-Biliary-Pancreatic Surgery, 108 Central Military Hospital said that before the transplant, patient H. was assessed for the donor's blood type antibody titer, then the antibody titer was adjusted, and desensitization treatment with the immunosuppressant drug Rituximab combined with plasma exchange 3 times. At that time, the antibody titer was 1/8, which is the safe value to perform a liver transplant for the patient.
On the morning of October 7, mother and daughter underwent the major surgery of their lives.
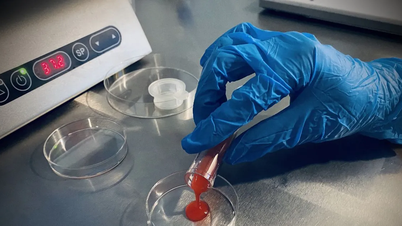
After intensive pre-transplant preparation, the liver transplant team performed laparoscopic surgery to remove the right liver graft from a living donor to transplant the liver into the female patient. The surgery lasted 8 hours.
Associate Professor, Doctor Vu Van Quang, Deputy Head of the Department of Hepato-Biliary-Pancreatic Surgery, 108 Central Military Hospital, said that this case had been operated on twice before, so there was an adhesion in the patient's abdomen, so when performing surgery, the adhesion had to be removed.
"The patient had many tumors in the liver, so care must be taken during surgery. The donor had abnormalities in the biliary tract. When performing the biliary anastomosis on the graft, care must be taken to avoid biliary leakage or stenosis," Dr. Quang shared.

Waking up after the transplant, H. thought of her mother first. A week after the transplant, Ms. Th. was allowed to visit her daughter. Both mother and daughter were moved and happy to see that both were recovering well. "Usually, we only saw each other when we called each other. Today, being able to go into the room with her and seeing her healthy, I am so happy that I can't describe it. I just hope that she can soon return to school like her friends," Ms. Th. said emotionally.
After a week of transplantation, the health of both the recipient and the donor was stable. The donor was discharged from the hospital after a week of transplantation. The recipient's health recovered well, the transplanted liver functioned normally, and he moved quickly.
Overcoming challenges in liver transplantation with incompatible blood types for patients
Increasing the source of donated organs is a problem for doctors in the work of mobilizing organ and tissue donation. Some measures have been implemented such as expanding the criteria for organ donation, donating organs from donors with cardiac arrest, using extracorporeal perfusion devices to preserve and restore organ function before transplantation, and donating organs from donors with ABO blood type incompatibility...
In the past, organ transplantation from ABO-incompatible living donors, including liver transplantation, was a contraindication due to the high risk of rejection, however, recent advances in immunomodulatory therapies have broken the barrier of ABO blood group compatibility, thereby increasing the source of organ donations for patients.
According to experts in the field of organ transplantation, currently, in some countries such as Taiwan (China), Japan and South Korea, liver transplantation from ABO-incompatible living donors is no longer a contraindication but has become a routine treatment method, with post-transplant results said to be equivalent to those of blood-type compatible transplants.

In Vietnam, ABO-incompatible donor transplantation has been performed in kidney transplant patients and in the pediatric liver transplant group. However, this technique has not yet been performed in adult liver transplantation.
"Although adult immunity is more complex than in children and the number of liver transplant patients is increasing, the source of donated livers is limited, so implementing incompatible blood type liver transplantation helps increase the chance of survival for people needing liver transplants," said Dr. Quang.
Source: https://nhandan.vn/du-bat-dong-nhom-mau-me-van-hien-mot-phan-la-gan-cuu-con-gai-post915814.html







![[Photo] Nhan Dan Newspaper launches “Fatherland in the Heart: The Concert Film”](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/16/1760622132545_thiet-ke-chua-co-ten-36-png.webp)



















![[Photo] General Secretary To Lam attends the 18th Hanoi Party Congress, term 2025-2030](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/16/1760581023342_cover-0367-jpg.webp)










































































Comment (0)