A 15-year-old boy was diagnosed with a hereditary kidney disease despite being otherwise healthy.
The male student from NHNA stated that he came for examination in stable health with no unusual symptoms. He had never previously undergone any tests to assess kidney function, such as abdominal ultrasound, urine tests, or blood creatinine measurements.
 |
| Individuals with a family history of polycystic kidney disease should undergo abdominal ultrasound screening. For those aged 15 to 39, the presence of three or more cysts in both kidneys may be a diagnosis. |
However, upon reviewing the family history, the doctor discovered a very clear genetic predisposition. Her maternal grandmother was diagnosed with polycystic kidney disease at age 60, and her mother was diagnosed at age 35. Due to negligence and lack of follow-up treatment, within just 5 years, her condition progressed to end-stage chronic kidney disease, requiring dialysis and awaiting a kidney transplant.
My maternal aunt (my mother's sister) was also diagnosed with the disease at age 33. My older sister, who is currently 17, has had an abdominal ultrasound but no signs of polycystic kidney disease have been detected at this time.
Based on information from the family tree and genetic risk factors, Dr. Nguyen Thi My Le, a specialist in Internal Medicine at MEDLATEC Go Vap Multi-Specialty Clinic, prescribed screening for hereditary polycystic kidney disease for A.
Abdominal ultrasound results revealed multiple cysts in both kidneys, with more than 7 cysts in the left kidney and more than 10 cysts in the right kidney, and the kidneys were larger than normal. Laboratory tests showed a creatinine level of 53.16, eGFR of 195 ml/min/1.73m², a normal urinalysis, and an albumin/creatinine ratio of 20.64, indicating that the patient's kidney function was not impaired.
Based on the abnormalities observed in the ultrasound images, the doctor diagnosed A with stage 1 chronic kidney disease, the earliest stage where kidney function is still normal and there are no clinical symptoms or extrarenal manifestations.
The doctor then ordered further screening tests to detect extrarenal manifestations of polycystic kidney disease, such as liver and pancreatic ultrasound to look for cysts, electrocardiogram and echocardiogram to detect early signs of valvular heart disease, coronary artery disease, or cerebral aneurysms.
Although medication wasn't immediately necessary, the patient was advised to take measures to protect kidney function as much as possible, such as drinking enough water to avoid dehydration, avoiding nephrotoxic medications without a doctor's prescription, limiting salt intake, and avoiding causes of urinary tract obstruction such as kidney stones.
At the same time, you also need to monitor the progression of the disease periodically through indicators such as renal volume using ultrasound or MRI, eGFR, proteinuria, albuminuria, and regularly check blood pressure as well as extrarenal manifestations such as liver cysts, cardiovascular disease, and cerebral aneurysms. If there are factors that accelerate the progression of kidney failure such as hypertension, proteinuria, hyperglycemia, or other glomerular diseases, early treatment is necessary.
The doctor also recommended that members of the patient's maternal family be screened for polycystic kidney disease, especially the two children of her maternal aunt. Although A's sister has not shown any symptoms on the current ultrasound, she still needs regular monitoring because the disease can have a late onset.
According to Dr. Le, polycystic kidney disease is a genetic disorder characterized by the appearance of multiple cysts in both kidneys, causing them to enlarge. Approximately 25% of cases are asymptomatic and therefore go undiagnosed. The disease progresses silently, with the number of cysts gradually increasing over time, leading to a gradual decline in kidney function.
If not detected and monitored early, the disease can progress to the end stage, requiring kidney replacement therapy such as hemodialysis, peritoneal dialysis, or kidney transplantation.
Furthermore, the disease can cause many other complications such as hypertension, kidney stones, urinary tract infections, back pain, hematuria, and especially extrarenal complications such as liver cysts, cerebral aneurysms which can lead to cerebral hemorrhage and cardiovascular diseases. Therefore, early screening provides an opportunity for timely treatment, slowing disease progression and improving the quality of life for patients.
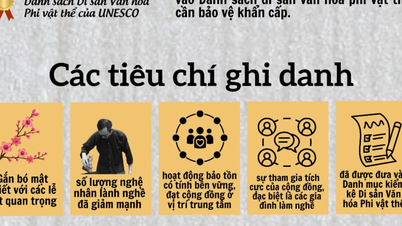
According to the International Society for Nephrology (KDIGO), individuals with a family history of polycystic kidney disease should undergo abdominal ultrasound screening. For individuals aged 15 to 39, the presence of three or more cysts in both kidneys may be a diagnosis.
In individuals aged 40 to 59, the standard is two or more cysts in each kidney. In addition to abdominal ultrasound, necessary tests for diagnosis and monitoring include complete blood count, electrolyte panel, BUN, serum creatinine, urinalysis, microalbuminuria/creatinineuria, electrocardiogram, echocardiogram, and ultrasound of the liver and pancreas.
Dr. Le emphasized that the kidneys have a very high compensatory capacity, so most kidney diseases, including polycystic kidney disease, progress silently. By the time symptoms appear, the damage is usually already severe. Therefore, people at high risk should proactively undergo screening for early detection and timely management.
Patients with gastrointestinal cancer are being treated with a new solution.
Hanoi Oncology Hospital announced that doctors from the General Surgery Department have successfully performed a total gastrectomy and esophageal reconstruction using a segment of the colon for a patient with a history of esophagectomy due to cancer.
According to the CT scan images, the patient showed severe damage to the gastric tube. After consultation, the doctors determined that the optimal treatment plan was to remove the entire gastric tube, perform radical lymph node dissection, and reconstruct the esophagus using a segment of the left colon.
According to Dr. Le Van Thanh, Deputy Director of the Hospital and Head of the General Surgery Department, this is a complex surgical technique requiring high-level coordination between the gastrointestinal surgery, anesthesia and resuscitation, and post-operative care teams.
Colonic reshaping not only requires ensuring adequate length and blood supply to the segment, but also taking into account anatomical changes caused by previous surgery.
During the surgery, the doctors brought the colon up to the chest and neck area, connecting it directly to the remaining part of the esophagus, completely replacing the digestive function of the removed stomach. This is one of the highly specialized surgical solutions that helps preserve the patient's natural ability to eat.
Following surgery, the patient recovered well, resumed eating and drinking early, maintained a stable overall condition, and was discharged after 8 days of inpatient treatment. Post-operative pathology results revealed stage III gastric duct cancer. The patient will now continue with adjuvant chemotherapy to improve overall treatment effectiveness and prolong survival time.
The surgery not only completely removes the malignant tumor but also maintains physiological digestive function, avoiding the need for bowel bypass surgery or prolonged use of alternative feeding methods. This is a key factor in improving the quality of life and the ability of cancer patients to reintegrate into the community after treatment.
Risk of recurrent stroke due to a large, mobile tumor in the heart.
Ms. Huong (64 years old) was admitted to the hospital experiencing fatigue upon exertion. Hospital examinations revealed a 11x4 cm myxoma located in her left atrium, migrating past the mitral valve. This poses a serious risk of embolism, recurrent stroke, or sudden death if not treated promptly.
A year ago, Ms. Huong suffered a stroke. Doctors suspected the cause was an embolism from the heart. Three months later, an echocardiogram revealed a tumor in the left atrium, suspected to be a myxoma. Doctors recommended early surgery, but her family hesitated because she had not fully recovered from the stroke.
In June of this year, during a routine health check-up, Ms. Huong underwent a cardiac ultrasound and discovered a large tumor. Without timely surgery, the tumor could cause pseudo-narrowing of the mitral valve by obstructing the valve opening, leading to blood clots, stroke, or sudden cardiac arrest due to obstruction of blood flow. Doctors held a consultation and decided on emergency surgery to remove the tumor and prevent the risk of sudden death.
The surgery was performed by Dr. Tran Thuc Khang, Deputy Head of the Cardiovascular Surgery Department, Cardiovascular Center. The team removed the entire myxoma tumor attached to the interatrial septum, made a wide excision around the base of the tumor to minimize the risk of recurrence, and simultaneously checked and reshaped the mitral valve and interatrial septum.
Post-operative pathology confirmed it was a benign tumor. One week after surgery, Ms. Huong recovered well, no longer felt tired when exerting herself, resumed normal activities, and continued to receive supportive post-operative treatment.
According to Dr. Khang, cardiac myxoma is a rare disease, accounting for only about 0.01-0.2% of all heart surgeries, of which 75% are benign tumors. The tumor usually appears in the left atrium, although in some cases it may be located in the right atrium or ventricle.
Although benign, myxomas can cause serious complications such as mechanical obstruction (in the mitral valve, left ventricular outflow tract), distant embolism (tumor fragments travel through the bloodstream causing blockages in the brain, limbs, or organs), local damage (causing mitral valve damage, conduction disorders), and even sudden death.
Patients may not have obvious symptoms. Some may experience systemic manifestations such as prolonged fever, weight loss, fainting, fatigue on exertion, or sudden death.
Therefore, doctors recommend that elderly people and those with abnormal cardiovascular symptoms should seek examination at specialized medical facilities for early diagnosis and timely treatment. Among these, echocardiography is a standard, simple, and effective method for early detection of cardiac myxoma.
Avoid the risk of facial paralysis by detecting parotid gland tumors and receiving appropriate treatment.
Mr. Toan (name changed), while undergoing examination at Tam Anh General Hospital in Ho Chi Minh City, was found to have a 4.5 cm parotid gland tumor that had spread to the deep lobe of the left parotid gland.
The biopsy results confirmed it was a benign tumor; however, its large size and location close to the 7th cranial nerve meant the case posed a high risk of facial paralysis if not treated properly.
According to Dr. Do Tuong Huan, a specialist in Breast and Head and Neck Surgery, the parotid gland is the largest salivary gland and has cranial nerve VII (facial nerve) running through it.
When adenomas grow large, especially extending to the deep lobes, they can compress and deform the facial nerve, making surgery more difficult and increasing the risk of nerve damage during and after the operation.
Given this situation, the doctor prescribed surgery to remove the tumor while preserving as much of the facial nerve as possible to prevent complications such as facial paralysis. The surgical team proceeded to expose the entire left parotid gland, locate the origin of the 7th cranial nerve, and sequentially separate the five branches passing through the gland to remove the superficial lobe. Then, accessing the deep lobe where the tumor was located, the doctors performed the procedure to separate and lift the facial nerve network, completely removing the deep lobe containing the tumor.
Following surgery, the patient experienced temporary mild paralysis of the facial nerve and the greater auricular nerve, but no dangerous complications were observed. The doctor predicted that neurological function would recover within a few weeks. Post-operative pathology results confirmed the tumor was benign.
The parotid gland is one of the body's three main salivary glands, alongside the submandibular and sublingual glands.
This gland is responsible for secreting large amounts of saliva into the oral cavity. The seventh cranial nerve, which controls the facial muscles, runs through the glandular tissue; therefore, any injury or surgery in this area must be carefully considered and performed with great caution.
Parotid gland tumors are a type of salivary gland tumor that usually develops slowly over many years, is painless, and the skin in the affected area remains smooth and does not become infiltrated.
The exact cause of the disease is unknown, but identified risk factors include viral infections, salivary gland stones, gene mutations, radiation exposure, and unhealthy lifestyles such as smoking, a high-fat diet, and foods high in cholesterol.
According to experts, the disease can occur in both adults and children, but if detected early and treated properly, the chances of recovery are very high.
People are advised that if they notice any unusual swelling or puffiness in the parotid gland area, difficulty chewing or swallowing, or a noticeable difference in sensation compared to the opposite side, they should quickly go to a specialized medical facility for examination.
Regular health checkups also play an important role in the early detection of abnormalities in the salivary glands and structures of the head, face, and neck.
Source: https://baodautu.vn/tin-moi-y-te-ngay-69-phat-hien-mac-benh-than-di-truyen-du-hoan-toan-khoe-manh-d379416.html





![[Photo] Closing Ceremony of the 10th Session of the 15th National Assembly](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F11%2F1765448959967_image-1437-jpg.webp&w=3840&q=75)
![[Photo] Prime Minister Pham Minh Chinh holds a phone call with the CEO of Russia's Rosatom Corporation.](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F11%2F1765464552365_dsc-5295-jpg.webp&w=3840&q=75)





































































































Comment (0)