
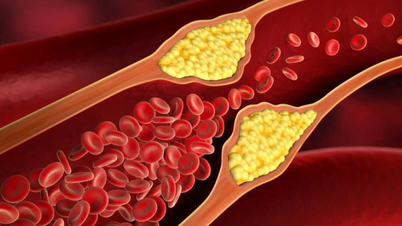
Itchy, dry, cracked skin can be a sign that you have diabetes - Illustration: AI
According to doctors at the Central Endocrinology Hospital, when blood glucose levels increase, the body will become dehydrated due to frequent urination and reduced blood flow to nourish skin tissue. At the same time, damage to peripheral nerves disrupts the activity of sweat glands, leading to prolonged dry skin and uncomfortable itching.
Dry, inelastic skin is prone to cracking, creating open wounds that may be just superficial scratches on the surface or may extend deep into the subcutaneous tissue. These wounds become a gateway for bacteria to enter, causing dermatitis, soft tissue infections, and even abscesses.
When the patient tries to scratch to relieve the itch, it will accidentally cause the skin to be scratched, torn and more difficult to heal - especially in the lower limbs where blood circulation is poor.
Below are some signs of itchy skin symptoms caused by diabetes.
1. Localized or diffuse itching
Common locations: hands, feet, calves, chest, back or areas with folds such as groin, armpits, neck. Localized itching can be caused by fungal infections, folliculitis, contact dermatitis. Generalized itching is often associated with neurological complications or long-term metabolic disorders.
2. Dry, peeling, cracked skin
This is an early and very common symptom in people with high blood sugar. The skin loses water, reduces sebum production, leading to dryness, flaking, a feeling of tightness and itching. It appears more clearly on the shins, elbows, or areas of skin that are rubbed frequently.
3. Itchy, tingling sensation
It is a sign related to peripheral nerve damage caused by long-term high blood sugar. Patients often describe "itching but not knowing where to scratch", or "itching like something is crawling under the skin".
This feeling often occurs in the hands and feet, and may be accompanied by numbness and loss of hot/cold sensation.
4. Itching with skin lesions
Itching may be accompanied by signs such as: red rash, blisters, pustules (due to bacterial or fungal infections). Dark, thickened skin (signs of acanthosis nigricans).
Clusters of small yellow nodules (xanthomatosis), often associated with dyslipidemia. Dark red, atrophic skin, often on the lower legs (diabetic fat necrosis).
5. Itching a lot at night
Is a typical sign of neurological complications. At night, when body temperature increases slightly and peripheral nerves function abnormally, the itching, burning, tingling sensation becomes intense, causing difficulty sleeping or prolonged insomnia.
6. Itching recurs many times and does not go away with treatment
If the patient has persistent skin itching, which goes away and then recurs despite treatment, it is a sign that: blood sugar is not controlled stably, there may be an underlying infection, and antifungal/antibacterial treatment is needed according to the regimen. Or chronic complications have appeared and are progressing.
In addition, another serious complication associated with itching and skin damage is necrobiosis lipoidica diabeticorum.
This condition usually appears on the lower legs with the initial manifestation being reddish-brown rashes with clear edges, hair loss in the center, smooth skin, and even visible veins under the skin.
If not detected and treated early, these damaged skin areas can progress to deep, oozing, painful ulcers that are difficult to heal, increasing the risk of infection and amputation.
Itchy skin in diabetic patients is not only a simple skin symptom but also a warning sign of internal disorders in the body.
When you have the above symptoms of itchy skin, you may have diabetes and need to go to a medical facility for timely diagnosis and advice.
Early recognition of typical signs, combined with good blood sugar control and proper skin care will help patients limit complications and improve quality of life.
Source: https://tuoitre.vn/da-kho-nut-ne-ngua-ngay-can-trong-mac-dai-thao-duong-20250818170027785.htm


![[Photo] Prime Minister Pham Minh Chinh and his wife meet the Vietnamese community in Algeria](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/19/1763510299099_1763510015166-jpg.webp)

![[Photo] General Secretary To Lam receives Slovakian Deputy Prime Minister and Minister of Defense Robert Kalinak](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/18/1763467091441_a1-bnd-8261-6981-jpg.webp)






































































































Comment (0)