On the afternoon of October 16, sharing about this case, doctors at the 108 Central Military Hospital (TWQD) said that in March 2023, NTH (15 years old) was diagnosed with a liver tumor, with complications of tumor rupture and had surgery. After that, he was transferred to the National Children's Hospital for examination and treatment, and had two embolization interventions.
In April 2025, the patient underwent the third embolization intervention at the 108 Military Central Hospital. However, the liver tumors continued to grow and increase in size. Therefore, the patient was indicated for a liver transplant.

Faced with the threat to her child's life, the mother decided to donate her liver to save her child. However, the mother and daughter did not have the same blood type (the child had blood type O, the mother had blood type B). For ABO incompatible liver transplantation, the most important issue is to reduce the amount of antibodies against A and/or B antigens in the recipient's serum to a safe level, so as not to cause excessive immune responses against the transplanted liver.
This is the second blood-type incompatible liver transplant the hospital has performed, so they have experience and have prepared carefully before the transplant.
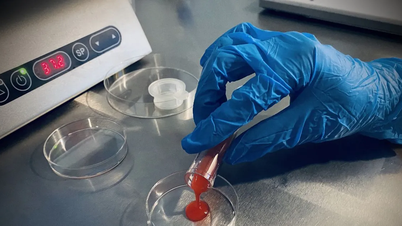
The liver transplant team performed laparoscopic surgery to remove the right liver graft from a living donor to transplant the liver into the female patient.
According to Associate Professor, Dr. Vu Van Quang, Deputy Head of the Department of Hepatobiliary-Pancreatic Surgery, 108 Military Central Hospital, the patient had undergone two previous surgeries and had many tumors in the liver, so there were adhesions in the abdomen and the adhesions had to be removed during surgery. For donors with abnormalities in the biliary tract, care must be taken to avoid biliary leakage or stenosis.
After 8 hours of surgery, the liver removal and transplant was successful. A week after the transplant, the mother was allowed to visit her daughter. Both mother and daughter were moved and happy to see that both were recovering well.

According to doctors, the mother was discharged from the hospital after 1 week. The child's health has recovered well, the transplanted liver is functioning normally, and he is moving quickly.
Previously, in 2023, the first incompatible blood type liver transplant was performed at 108 Military Central Hospital, when a grandmother donated her liver to save her 15-year-old granddaughter who had hepatocellular carcinoma on the background of cirrhosis. The incompatible blood type liver transplant was successful, opening up a lot of hope for life for patients who need liver transplants but lack donor organs.
In the past, transplantation from living donors with ABO blood type incompatibility, including liver transplantation, was a contraindication due to the high risk of rejection. However, recent advances in immunomodulatory therapies have broken the barrier of ABO blood type compatibility, thereby increasing the availability of organ donations for patients.
Currently, in some countries such as Taiwan (China), Japan and Korea, liver transplantation from ABO-incompatible living donors is no longer a contraindication but has become a routine treatment method, with post-transplant outcomes said to be equivalent to those of blood-type compatible transplants.
In Vietnam, organ transplantation from ABO-incompatible blood sources has been performed on kidney transplant patients and on liver transplant groups in children, but has not yet been performed in liver transplantation in adults.
Although adult immunity is more complex than in children and the number of liver transplant patients is increasing, the supply of donated livers is limited, so the implementation of allogeneic liver transplantation helps increase the chance of survival for people with end-stage liver disease who need a liver transplant to save their lives.
Source: https://cand.com.vn/y-te/me-bat-dong-nhom-mau-hien-gan-cuu-song-con-gai-17-tuoi-i784831/




![[Photo] Nhan Dan Newspaper launches “Fatherland in the Heart: The Concert Film”](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/16/1760622132545_thiet-ke-chua-co-ten-36-png.webp)






















![[Photo] General Secretary To Lam attends the 18th Hanoi Party Congress, term 2025-2030](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/16/1760581023342_cover-0367-jpg.webp)







![[Video] TripAdvisor honors many famous attractions of Ninh Binh](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/10/16/1760574721908_vinh-danh-ninh-binh-7368-jpg.webp)
































































Comment (0)