Having red, scaly patches on the scalp, waist and lower legs for many years, recently, 24-year-old NVH felt pain in his left knee and ankle. He went to the doctor and was diagnosed with psoriatic arthritis - a disease that can cause deformity, joint destruction and even disability.
Knee and ankle pain due to psoriatic arthritis
Mr. NVH (24 years old, Nghe An ) came to MEDLATEC General Hospital for examination due to symptoms of pain in the left knee and ankle.
Through questioning, Mr. H. said that the joint pain appeared about 4 days before being admitted to the hospital, and he had no history of trauma. In particular, the patient shared that about 4 years ago, the scalp area appeared red, then spread to the waist, both legs, peeled a lot, not itchy, the patient bought Clobetasone to apply and it got better and continued to maintain it until now.
After the clinical examination, MSc. Dr. Trinh Thi Nga - Orthopedic Specialist, MEDLATEC Healthcare System found that the patient had Cushing's phenotype, obesity level II; red skin with clear boundaries, thick skin, white flaking on the scalp, waist, elbows; pitted nails; small red skin on both elbow folds, no skin thickening, thin flaking surface, no blisters. Doctor Nga preliminarily diagnosed the patient with Arthritis - Psoriasis monitoring - Obesity level II - Cushing's syndrome caused by drugs.
To confirm the diagnosis, Dr. Nga ordered the patient to perform the necessary tests and imaging diagnostics on bones, joints and endocrine. At the same time, because the patient had skin lesions, Dr. Nga advised the patient to visit the Dermatology Department to have a specialist examine and evaluate the condition of the disease. After the examination, Dr. Tran Thi Thu - Dermatology Specialist, MEDLATEC Healthcare System advised the patient to do an additional skin biopsy to evaluate the condition of the disease.
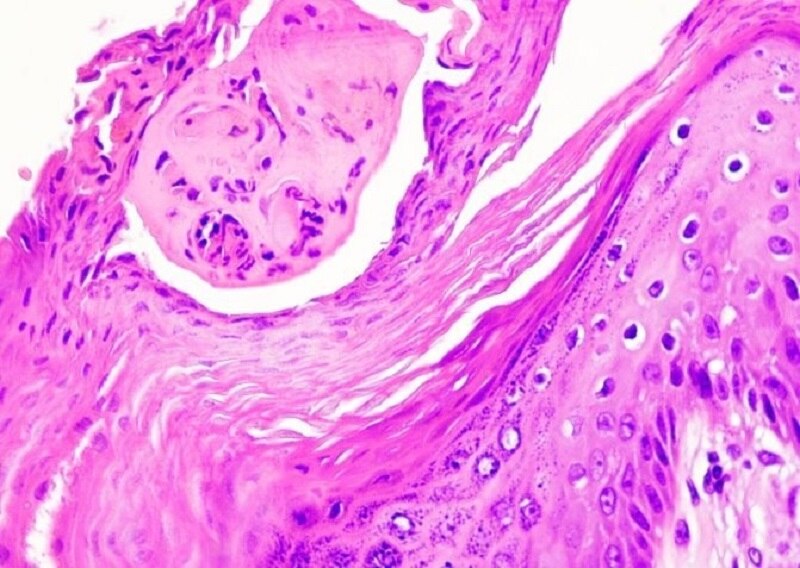
X-ray results revealed a radiopaque nodule at the left tibial tuberosity, left knee ultrasound showed a small amount of joint fluid (5.2mm) and a small fluid collection under the patellar ligament attachment (3x6mm). In addition, fresh smear fungal test (both arms) showed positive results for yeast, the image strongly suggested Malassezia furfur - the fungus that causes pityriasis versicolor, the histopathological test results were consistent with psoriasis.
Image of contrast nodule at the patient's left tibial tuberosity
Histopathological examination image consistent with psoriasis
Based on the results, the doctor diagnosed Psoriatic Arthritis - Moderate Plaque Psoriasis - Pityriasis Versicolor - Grade II Obesity - Monitoring of drug-induced adrenal insufficiency - Monitoring of hypothyroidism. Dr. Nga advised the patient to stop using Clobetasone topical medication and pay attention to proper daily hygiene and prescribed appropriate treatment for the patient's condition.
Psoriatic arthritis can be disabling.
Psoriatic arthritis (PsA) is a chronic inflammatory joint disease associated with psoriasis of the skin. The disease can occur at any age but is most common in people aged 40-50, with an equal ratio of men to women. The affected organs are diverse, including: spine, shoulder-elbow-wrist-hand-hip-knee-ankle joints, skin, nails and associated diseases such as osteoporosis, uveitis, intestinal damage, cardiovascular disease. In particular, the disease is chronic and progresses in episodes, causing damage and loss of function of joints and spine, which can lead to disability.
Psoriatic arthritis occurs in about 10-30% of patients with psoriasis, about 80% of arthritis cases appear after psoriatic lesions, 15% of cases appear simultaneously, and 10% of arthritis cases appear before psoriatic lesions. The disease is often diagnosed late or difficult to diagnose.
Elbow joint area with arthritis related to psoriasis (Illustration)
Psoriatic arthritis cannot be cured, what should be done to prevent it?
Russian doctor said: “ There is no radical treatment for psoriatic arthritis, treatment methods can only relieve symptoms and limit the development of inflammation. Some treatments include: Using non-steroidal anti-inflammatory drugs (NSAIDs), classical slow-acting anti-rheumatic drugs such as Methotrexate, Sulfasalazine... or biological forms (TNF-α inhibitors, IL-17 inhibitors, IL-23 inhibitors..., intra-articular corticosteroid injections if not responding to NSAIDs, surgery if joint damage is severe, causing adhesion, deformity, loss of joint function ”.
Doctors recommend that patients change their lifestyle to prevent the risk of disease as well as reduce dangerous complications caused by the disease. Patients can:
- Change your daily activities to reduce damage to your joints;
- Follow an anti-inflammatory diet;
- Regular exercise improves joint condition;
- Avoid stress, prolonged stress causes pain flare-ups, making the disease worse;
- Regular health check-ups every 6 months if there are risk factors: Genetics, immunity and environment;
- Psoriatic arthritis is not a rare disease, but because of its easily confused symptoms, patients can be overlooked and leave many negative effects on the body due to lack of timely treatment.
MEDLATEC has full facilities for diagnosing and treating psoriasis. Call MEDLATEC Healthcare System via hotline 1900 56 56 56 to get your questions answered and schedule a quick specialist appointment.






























![[Photo] National Assembly Chairman attends the seminar "Building and operating an international financial center and recommendations for Vietnam"](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/7/28/76393436936e457db31ec84433289f72)

































































Comment (0)