Overnight life revived from donated liver
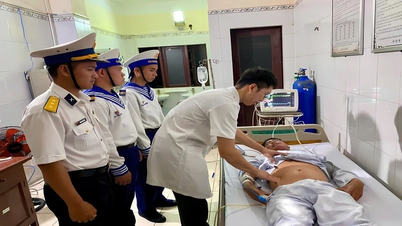
On the afternoon of June 23, 108 Military Central Hospital received a notice from the National Organ Transplant Coordination Center about a case of a brain-dead patient at E Hospital due to a traffic accident.
The patient’s family, overcoming the pain of loss, decided to donate organs to save the lives of others. This is a noble act, demonstrating compassion and spreading a message of humanity in the community.
There was no more time for a centralized consultation. On the evening of June 23, upon receiving information that there was an organ donated from a brain-dead donor, the Director of the 108 Central Military Hospital urgently convened a liver transplant subcommittee for an online consultation, urgently performing a liver transplant to save the life of a young soldier with liver cancer.
Doctors perform liver transplant surgery for a patient. (Photo: BVCC). |
As soon as the donated liver was coordinated, the professional team at the Hepatobiliary and Pancreatic Surgery Department quickly identified the transplant recipient as a soldier working in the 12th Army Corps, suffering from multifocal hepatocellular carcinoma on the background of cirrhosis due to hepatitis B, a dangerous condition requiring an emergency liver transplant.
Due to the unusual developments in the organ recovery process, the ability to maintain the quality of the donated liver until the morning of June 24 is very difficult. In the face of the urgent situation, that same evening, Major General, Professor, Dr. Le Huu Song, Director of the Hospital, decided to convene an online meeting of the liver transplant subcommittee to deploy urgent steps.
Associate Professor, Dr. Le Van Thanh (Acting Director of the Institute of Digestive Surgery, Head of the Department of Hepatobiliary and Pancreatic Surgery) led the liver removal team at E Hospital. The left lobe of the liver was coordinated for a child patient at Vinmec Hospital, while the right lobe of the liver was brought to the 108 Military Central Hospital at 2:00 a.m. on June 24 for transplantation to the patient.
The liver transplant team worked through the night. After 4 hours of intense surgery, the transplant was successfully completed. The patient was fully conscious after the surgery and was transferred to the Department of Surgical Resuscitation and Organ Transplantation for further monitoring and treatment.
Liver transplantation is a complex major surgery that requires careful preparation at every stage, from assessing the recipient's suitability index, planning for risks, to mobilizing a multidisciplinary team to coordinate. Every detail must be performed meticulously and accurately.
Dr. Vu Ngoc Tuan (Hepatobiliary and Pancreatic Surgery Department) shared that each step of preparation is a race against time. We are always aware that any mistake is a mistake to the donor. Therefore, everyone works with the highest spirit and concentration.
After each successful transplant, there is a deep gratitude to the donor and their family - the people who chose to sow hope in times of pain. It is this humane act of organ donation that gives a chance to live to those who are on the brink of life and death.
Major General, Professor, Dr. Le Huu Song, Director of 108 Military Central Hospital, emotionally shared that organ transplantation is a matter of expertise, but organ donation is a matter of conscience and humanity. Brain-dead organ donors not only leave this life but also leave behind a part of their body to continue living and contributing in another person's body. We would like to express our gratitude for this noble gesture.
Each successful transplant is not only a medical miracle but also a symbol of love, a testament to the power of humanity, where death is no longer the end, but becomes a new beginning for fragile lives.
Warning of myocardial infarction in young people
Mr. Lam, 33 years old, is obese level 2 (BMI = 35.4) and has felt a sharp pain in his left chest many times but subjectively ignored it, thinking it was just a normal sign. However, one night, he suddenly had a severe chest pain, spreading to his left arm and under his chin, accompanied by sweating. He was taken to the emergency room at Tam Anh General Hospital in Ho Chi Minh City by his relatives in critical condition.
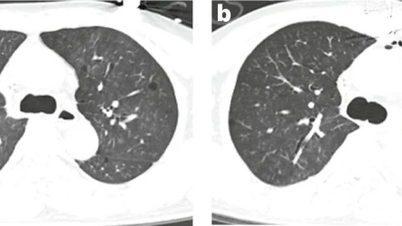
At the Interventional Cardiology Center, doctors determined that he had a non-ST elevation myocardial infarction (NSTEMI), a type of heart attack that occurs when a coronary artery is partially blocked. Coronary angiography results showed that he had a 99% narrowing of the anterior interventricular artery, one of the important locations that feeds the heart.
Immediately, Dr. Nguyen Van Duong and his team intervened by inserting a guidewire through the blockage, dilating the balloon and placing a 3.0×28mm stent under the guidance of intravascular computed tomography (OCT). After 30 minutes, blood flow was restored, pain was significantly reduced, hemodynamics were stable and the patient was discharged after 5 days of monitoring.
According to Dr. Duong, myocardial infarction is rapidly becoming younger. Previously, the disease was common in people over 45 years old, but now there are more and more cases under 35 years old, even people under 30 years old are in critical condition. Statistics show that the rate of myocardial infarction in the 30-34 age group is 12.9/1,000 in men and 2.2/1,000 in women.
Notably, symptoms in young people are often atypical. In addition to severe chest pain, patients may feel tired, have difficulty breathing, sweat, feel nauseous, have epigastric pain, or faint.
These symptoms are easily confused with digestive disorders or mild problems, leading to delayed diagnosis and increased risk of complications such as arrhythmia, acute heart failure, pericarditis or sudden death.
Experts recommend that young people should not be subjective with unusual signs of the body, especially chest pain, shortness of breath or prolonged fatigue.
In addition to cardiovascular diseases such as myocardial infarction and stroke, proactive periodic screening for dangerous diseases such as cancer is also increasingly receiving attention.
With the remarkable development of modern diagnostic imaging technology and intervention techniques, many dangerous diseases can be detected early, even when there are no obvious symptoms, thereby improving treatment effectiveness and long-term quality of life for patients.
Robots support cancer cutting with high efficiency
Mr. HND, 80 years old, residing in Ho Chi Minh City, was hospitalized with symptoms of hematuria, prolonged painful urination and pain in the lower abdomen. After examination at the Department of Urology - Center for Urology - Nephrology - Andrology, Tam Anh General Hospital, Ho Chi Minh City, doctors discovered that he had bladder cancer with a 4 cm malignant tumor that had deeply invaded the muscle layer and spread to the left pelvic area.
According to Associate Professor, Dr. Vu Le Chuyen, Director of the Center, the patient was elderly and had many underlying diseases such as high blood pressure and diabetes, so he was not healthy enough to endure a long open surgery.
Therefore, the doctor recommended surgery to remove the entire bladder to prevent metastasis and increase the patient's chance of long-term survival. After being consulted about surgical options, Mr. D. agreed to choose laparoscopic surgery with the support of the Da Vinci Xi robot, a minimally invasive method, reducing pain, shortening recovery time and suitable for the elderly.
With the support of the Da Vinci Xi robotic system, medical experts performed surgery to remove the patient's entire bladder, seminal vesicles, prostate, and bilateral pelvic lymph nodes.
The robot with four flexible mechanical arms has helped the doctor reach deep into the narrow pelvic area, operate precisely, cut, burn, stop bleeding meticulously, without causing significant bleeding. This is one of the outstanding advantages of the robot compared to conventional laparoscopic surgery, especially when intervening in deep areas, difficult to operate by hand.
After removing the bladder, doctors open the two ureters to the skin to drain urine. Associate Professor, Dr. Chuyen said that if the patient is young and the tumor has not spread to the urethra, the bladder can be reconstructed using a piece of small intestine.
However, Mr. D.'s case was not suitable for this technique because the tumor had invaded the urethra. After surgery, the patient recovered quickly, had little pain, and was discharged after only 3 days.
During the first 1-3 months, the patient needs to be closely monitored to ensure effective urinary drainage and to avoid complications. After recovery, Mr. D. continued chemotherapy at the hospital's Oncology Department.
Malignant bladder cancers are divided into two groups: superficial, which is confined to the mucosal layer, and invasive, which has penetrated the muscular layer. According to the American Cancer Society, approximately 84,870 new cases of bladder cancer are diagnosed each year, resulting in approximately 17,420 deaths.
The 5-year survival rate depends largely on the stage at which the disease is detected. In the early stages, effective treatment can be achieved by surgery or local bladder chemotherapy. When the cancer has invaded the muscle layer, it is necessary to remove the entire bladder, combined with systemic chemotherapy before or after surgery, depending on the patient's condition.
Bladder cancer often presents with nonspecific urinary symptoms such as hematuria, painful urination, frequent urination, pelvic or lower back pain. This makes the disease prone to late diagnosis.
Some risk factors include cigarette smoking, exposure to toxic chemicals, chronic cystitis, a history of pelvic radiation therapy, use of certain chemotherapy drugs, advanced age (over 55 years), and genetic factors.
To prevent bladder cancer, doctors recommend building a healthy lifestyle, not smoking, drinking enough water, exercising regularly, avoiding exposure to chemicals and having regular health check-ups for early detection and timely intervention.
Thinking it was gastritis, a 13-year-old girl almost suffered complications from acute appendicitis.
Huyen (13 years old) had a dull stomachache that lasted for two days, accompanied by diarrhea and vomiting. Her family thought it was gastritis so they took her to the doctor. After being diagnosed with gastritis and prescribed medication to take at home, her stomachache did not improve but became more severe. Her family immediately took her to the emergency room at Tam Anh General Hospital in Ho Chi Minh City.
Here, MSc. Dr. Ton Thi Anh Tu (Department of Pediatric Surgery) said that the results of the blood test showed that the white blood cell count increased to 16,320G/L (normally below 10G/L), of which neutrophils accounted for 75.2%, the CRP index reflecting inflammation was up to 48mg/L (normally below 5).
Abdominal ultrasound showed a 12mm appendix with surrounding fat infiltration, a clear sign of acute appendicitis. Fortunately, the appendix had not ruptured or become necrotic. Huyen had her appendix removed by a laparoscopic surgical team that night and was discharged safely after two days of treatment.
According to Dr. Tu, acute appendicitis is one of the most common causes of surgical emergencies in children. The appendix is a small, finger-shaped segment of intestine located at the beginning of the cecum. When inflamed, especially in the early stages, the symptoms are easily confused with other digestive diseases such as gastritis, enteritis, adnexitis or Meckel's diverticulitis.
Doctors analyze that gastritis is often caused by viruses such as Rotavirus, Norovirus or bacteria such as E.coli, Salmonella through unsanitary food and water. Symptoms often include dull pain in the epigastric region, vomiting, diarrhea, accompanied by a mild fever.
Meanwhile, acute appendicitis often begins with a dull pain around the navel or epigastric region, after a few hours gradually moving down to the right iliac fossa, where the appendix is located and the pain increases significantly when coughing, sneezing, moving or pressing. The disease may be accompanied by loss of appetite, nausea, fever and sometimes diarrhea.
Appendicitis, if not detected and operated on promptly, can lead to dangerous complications such as ruptured appendix, causing peritonitis, a severe abdominal infection that can be life-threatening.
Doctor Tu recommends that when children show signs of prolonged abdominal pain, especially pain localized in the lower right abdomen, accompanied by fever, nausea or diarrhea, parents should take their children to the hospital or medical facility for an accurate diagnosis.
Never give your child painkillers or antibiotics without consulting a doctor as this may mask the symptoms and make diagnosis difficult. Also, do not apply heat to the abdomen as this may increase the rate of inflammation and the risk of a ruptured appendix.
Source: https://baodautu.vn/tin-moi-y-te-ngay-266--xuyen-dem-hoi-sinh-su-song-tu-la-gan-hien-tang-d314338.html








![[Photo] Closing of the 13th Conference of the 13th Party Central Committee](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/08/1759893763535_ndo_br_a3-bnd-2504-jpg.webp)





























































































Comment (0)