According to information from Monash University, a study from Monash University (Australia) has just proven that, with the right support, the human body itself can become a powerful "warrior" against cancer, bringing hope for new generation immunotherapies.
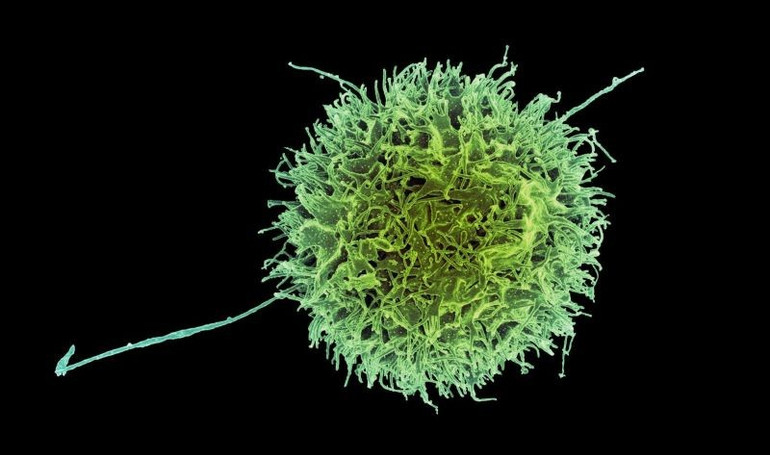
The human body has a natural defense mechanism against cancer, a growth factor called IL-15. This factor stimulates the production of immune cells, including Natural Killer (NK) cells, which help detect and destroy cancer cells as soon as they form.
However, cancer cells are constantly evolving and developing sophisticated mechanisms to “disable” the immune system, even in an IL-15-rich environment. One approach that seems to be effective is to give patients drugs that activate IL-15 receptors on immune cells. However, these therapies cause severe toxicity because they activate the immune system throughout the body, rather than just at the tumor, leading to many severe side effects.
Now, a new study conducted by Monash University and biotechnology company oNKo-Innate (Melbourne, Australia) is opening up a promising direction for cancer treatment.
Accordingly, the research team discovered a gene that can be "turned off" in NK cells, making these cells particularly sensitive to endogenous IL-15, thereby promoting the ability to destroy cancer more effectively.
The study, conducted by Professor Nick Huntington (Monash Institute of Biomedical Research) and colleagues, was published in the international journal Cancer Cell. This study shows that when this gene is removed from human NK cells, even small amounts of IL-15 are enough to strongly activate the ability to kill cancer, helping to slow the growth of colorectal cancer in preclinical models.
Interestingly, this gene encodes an enzyme, meaning it can be inhibited with small-molecule drugs. In fact, a drug being tested to treat myelodysplastic syndrome has been shown to interfere with the same molecular pathway, helping to kill cancer cells.
“This offers hope for the development of more specific, safer drugs for use in cases where immunotherapy is not optimal and requires further enhancement of the anti-cancer immune response,” Professor Huntington said.

In colorectal cancer patients, tumors often secrete more IL-15 than healthy tissue. However, cancer cells can also mutate the IL-15 gene to evade the immune system - a factor often associated with the risk of recurrence and poor prognosis. Increasing the sensitivity of immune cells to endogenous IL-15 helps to trigger a strong response at the tumor site, while limiting the effect on tissues where IL-15 is almost non-existent.
The team used CRISPR technology to screen and identify genes that increase the sensitivity of immune cells to growth factors. The results showed that two genes could be knocked out in cell therapies, or inhibited with drugs, thereby improving the cancer-killing effectiveness of NK cells.
According to Mr. Jai Rautela, CEO of oNKo-Innate, this discovery can be combined with current immunotherapies such as immune checkpoint inhibitors to create a synergistic effect.
“Drugs that enhance IL-15 signaling could provide an additional layer of defense, reinforcing the immune response in advanced tumors,” he said. “This is evidence that a deeper understanding of immunology can lead to breakthroughs in solving difficult biological problems such as IL-15, and pave the way for a new generation of immunotherapies.”
Source: https://nhandan.vn/dai-hoc-monash-phat-hien-co-che-tang-suc-manh-cho-te-bao-diet-ung-thu-post887482.html
























![[Video] From advertising to printing – the thousand-year journey of news](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/6/20/ddaafc5481924a59affdca906d9bbbfd)



![[Photo] The 9th Congress of the Party Committee of the Office of the President, term 2025-2030](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/6/20/78e7f27e8c4b4edc8859f09572409ad3)
























![[Maritime News] Wan Hai Lines invests $150 million to buy 48,000 containers](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/6/20/c945a62aff624b4bb5c25e67e9bcc1cb)













































Comment (0)