Ho Chi Minh City To perform awake brain surgery, the most difficult thing for the anesthesia team is to control the patient's vital signs and keep the patient awake enough without feeling pain.
On August 26, Master, Doctor, CKII Luu Kinh Khuong, Head of the Department of Anesthesia and Resuscitation, who directly performed anesthesia on the patient who had brain surgery a week ago, said the above, adding that "this is a surgery that requires high techniques".
The patient who underwent wake-up surgery was Mr. Ngoc (42 years old, living in Binh Duong ) who was in the emergency room due to a stroke and left hemiplegia. According to Master, Doctor, CK2 Chu Tan Si, Head of the Department of Neurosurgery, Neurology Center, Tam Anh General Hospital, Ho Chi Minh City, the brain CT scan results showed a cerebral hemorrhage in the right hemisphere. Blood pressure at the time of admission was high (170/110 mmHg).
Doctors held an emergency consultation, adjusted blood pressure to the allowable threshold, and prescribed early brain surgery with an artificial intelligence (AI) robot.
"Awake surgery for hemorrhagic stroke when the patient is still conscious, able to communicate, and able to move is much more difficult than traditional surgery under general anesthesia," said Dr. Si. In return, doctors can better assess and control neurological, motor, and language functions during and immediately after surgery.

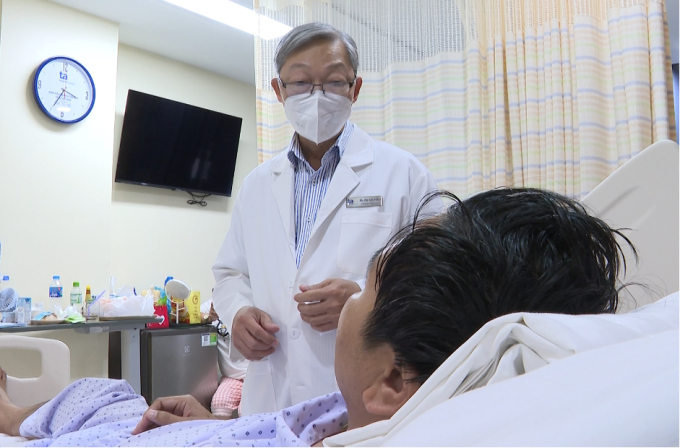
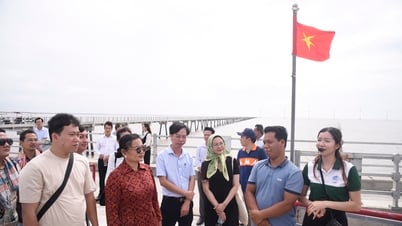
Doctors consult with patient Ngoc. Photo : Tam Anh Hospital
Dr. Khuong said the difficulty is to anesthetize effectively and with the right technique so that the patient is awake enough but still does not feel pain during brain surgery. The goal is to ensure that the patient lies still and cooperates throughout the surgery, avoiding agitation, movement, and convulsions that can lead to brain edema and dangerous cervical spine injuries. To do this, the anesthetic dosage must be carefully calculated and flexibly adjusted according to the requirements of the surgery and the patient's actual progress and reactions.
Patients are also given anesthetics to control heart rate, respiration, blood pressure, and SpO2. The doctor uses the Entropy device to monitor the depth of sedation when necessary to put the patient to sleep to avoid deep sleep leading to respiratory and airway reflex inhibition, hypoxia, and cardiac arrest.
First, the doctor anesthetizes the patient's entire scalp, using an ultrasound machine to identify and block the 12 nerve branches that control the head area. When the scalp is cut, the patient is still conscious and able to talk. When preparing to drill the skull and open the dura mater, the doctor adds anesthetic to help the patient feel sedated, "comatose" enough, without stimulation or pain.
The anesthetic only works well on the scalp, while the patient's skull and dura mater have many pain receptors. The team then reduces the amount of anesthetic so that the patient is awake and can interact while the hematoma is removed.

Doctor Khuong (dark green shirt) monitors the surgery and the patient's reaction during awake surgery. Photo: Tam Anh Hospital
To ensure success, before the actual surgery, the surgical team simulates on the computer to choose a safe approach to remove the hematoma, avoiding collisions that damage the nerve fiber bundles. The patient is scanned with a 3 Tesla MRI, DTI nerve fiber bundle scan, and the data is fed into the specialized software of the AI brain surgery robot to analyze the optimal access to remove the hematoma. The robot helps the doctor clearly see the hematoma, nerves, and healthy brain tissue on the same 3D image, thereby avoiding damage to the nerve fiber bundles and leaving sequelae for the patient.
The actual surgery followed the same surgical path as previously simulated, according to Dr. Khuong. The patient moved and talked during the surgery so that the doctor could assess neurological function and level of interaction.
After 30 minutes, the doctor removed all the blood clot, about 50 ml. The surrounding brain tissue and nerve fiber bundles were preserved. The patient was alert, recovered his health, and communicated well after 6 days of treatment. He continued to do physical therapy to improve his hemiplegia.
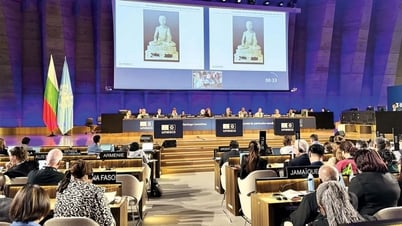
Doctor Tan Si visits a patient after surgery. Photo: Provided by the hospital
Dr. Tan Si added that the longer a stroke causes bleeding in the brain, the more dangerous it becomes. In addition to the blood clot causing space and compressing the nerve structure, after only 4 hours of brain hemorrhage, the blood clot begins to react inflammatoryly, producing cell toxins, damaging surrounding brain cells, damaging the blood-brain barrier, causing harm to the remaining brain cells.
The patient needs emergency surgery within the first 24 hours (later is less effective). It is best to have emergency surgery within the first 8 hours of signs of a hemorrhagic stroke because after a stroke, two million brain cells die every minute. The sooner the hematoma is resolved, the less damage is done and the higher the chance of survival and recovery.
Peaceful
* Patient name has been changed
| Readers ask neurological questions here for doctors to answer |
Source link





















































































![[Infographic] In 2025, 47 products will achieve national OCOP](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/7/16/5d672398b0744db3ab920e05db8e5b7d)







Comment (0)