When detecting a child suspected of being infected or infected with COVID-19 , parents need to calmly determine the severity of their child's illness.
If a child has mild COVID-19, home treatment is key to ensuring that the child receives good care from the family, has minimal psychological impact on the child, and limits unnecessary medical overload. The risk of contracting viruses and other diseases from the hospital is also reduced.
1. For infants and breastfeeding mothers
This is a group of children where the role of mothers is extremely important in directly caring for and closely monitoring the children.
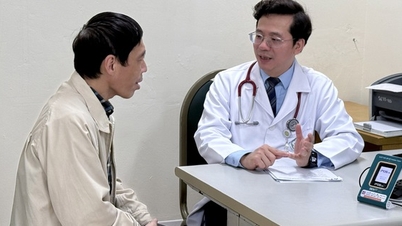
- In addition to fever-reducing methods, Associate Professor, Dr. Tran Minh Dien - Director of the National Children's Hospital, noted that parents need to give their children regular water and electrolyte drinks. Signs of dehydration include little urination, yellow, concentrated urine, and dry lips.
Electrolyte water needs to be mixed in the correct dosage. After giving it to your child, parents should monitor him day and night. After rehydration, if he urinates more frequently, is clearer, and his lips are not dry, then you can rest assured .
How to drink: 15 - 20 minutes/time, a few spoons each time.
- Feed your baby gently and divide the feedings and meals into smaller and more frequent ones. Do not force your baby to eat a lot at once, so that the baby can absorb more easily.
" Do not drink too much orange juice or fruit juice as it can cause vomiting and bloating " - expert Tran Minh Dien noted that if children cough, herbal cough syrups can be used to reduce symptoms.
- Children do not need to be taken to the hospital if parents ensure close monitoring of whether the child plays well, eats and drinks enough, and responds to fever-reducing medication and is alert. If the above conditions improve within 24-48 hours, the child can continue to be cared for at home.
Breastfeed your baby in small portions and closely monitor your baby's symptoms to promptly reduce fever and rehydrate (Photo: Internet)
2. Note when children 2-6 years old with COVID-19 have convulsions due to high fever
- Older children who have gone to school are able to protect themselves and express symptoms, and have a better sense of their body. However, parents still need to pay special attention to assessing fever both day and night, giving children fever-reducing medicine when the fever is above 38.5 degrees Celsius, and monitoring changes for 4 to 6 hours continuously by measuring the temperature.
- In children from 2 to 6 years old, high fever can cause convulsions when the temperature increases rapidly in a short period of time.
If the child has a seizure:
- Parents must be really calm and call for help from people around.
- Place the baby on a hard, flat surface, with the head slightly tilted back and to one side;
- Do not put anything in the baby's mouth to avoid causing tongue fall or difficulty breathing;
- Do not rush to hug or pick up the baby.
Remove some of the child's clothes, take the temperature, and give the child a suppository to reduce the fever.
Use a warm towel to wipe the neck, armpits, and groin and continue to monitor the child's condition. Usually, a simple febrile seizure only lasts about 1-2 minutes.
If the baby's lips and limbs are warm and pink afterwards, we can be completely reassured.
Parents need to stay calm and pay attention to instructions on how to handle high fever convulsions in children (Photo: Internet)
3. If the child's symptoms become more severe and persist, take the child to the nearest medical facility.
Most children can recover on their own after 1-2 weeks if properly cared for. However, there are many cases where the condition becomes severe and requires immediate medical intervention to avoid dangerous complications.
When your child shows any unusual symptoms other than the usual ones, parents should take their child to the nearest medical facility for timely treatment.
In particular, children with underlying diseases such as: premature birth, low birth weight, chronic lung disease, asthma, cancer, chronic kidney disease, organ transplant, diabetes, cardiovascular disease, neurological disease, hematological disease, systemic disease, immunodeficiency, being treated with corticosteroids or immunosuppressants... need to be given more attention, protection, and closer monitoring by specialists.
Source: https://suckhoedoisong.vn/giam-doc-bv-nhi-trung-uong-tu-van-cach-cham-soc-tre-mac-covid-19-tai-nha-169220223162609074.htm





![[Photo] Panorama of the 2025 Community Action Awards Final Round](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/15/1763206932975_chi-7868-jpg.webp)
![[Photo] General Secretary To Lam receives Vice President of Luxshare-ICT Group (China)](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/15/1763211137119_a1-bnd-7809-8939-jpg.webp)

![[Photo] Prime Minister Pham Minh Chinh meets with representatives of outstanding teachers](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/15/1763215934276_dsc-0578-jpg.webp)
























































































Comment (0)