Herpes zoster is a common disease in the elderly, especially those with underlying diseases or immunodeficiency, with the risk of serious complications if not treated promptly.
A typical case is that of Mrs. HTP (73 years old, Hanoi ) who had blisters on her left flank and abdomen, accompanied by a burning, stinging pain that lasted for a long time. Initially, her family thought she had “shingles” so they applied folk remedies such as applying green beans, but the condition got worse. The blisters spread, causing severe pain, making her tired, sleepless and having headaches for many days. When she was hospitalized, she was diagnosed with shingles with severe skin damage.
Or like Mr. TVS (70 years old, living in Long An province) was hospitalized with many pustules on the skin behind his head and back.
Taking the medical history, the patient said that he had previously had a throbbing pain in the back of his head, accompanied by the appearance of many blisters. Following the advice, he went to a shaman in the neighborhood to have his "drawing done". For 3 consecutive days, the shaman burned incense, drew with Chinese ink around the blister area, and applied tamanu oil. However, his pain did not subside, and the blisters became pus-filled, more painful, causing fever and discomfort.
Doctors recommend that when there are early signs of shingles such as burning pain, red rash or blisters on the skin, patients should go to the doctor early for timely diagnosis and treatment, avoiding the risk of dangerous complications.
What is shingles?
Shingles is a skin infection caused by the Varicella zoster virus (VZV), which attacks the skin and nerves. It is also called shingles or zoster. VZV is also the virus that causes chickenpox. After a person has had chickenpox and recovers, some of the Varicella virus can remain in the body in a latent state without causing disease.
This latent state can last for months or years and the VZV virus resides in nerve ganglia. When there are favorable conditions such as immunodeficiency, mental stress, or physical weakness, overwork leading to reduced body resistance... then this virus can reactivate.
VZV virus reproduces and spreads along sensory nerve pathways, damaging the skin and nerves, thereby causing the symptoms and signs of shingles.
2. Symptoms
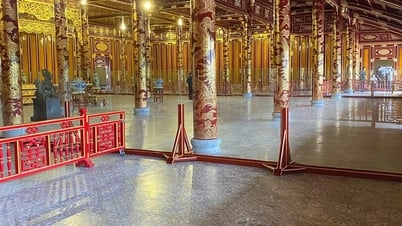
A patient with shingles suffered a severe infection due to using the "drawing" method. (Photo: VNA)
When suffering from shingles or complications of shingles, the symptoms often manifest as pain and discomfort:
Pain, burning, or tingling in the affected skin areas or shingles scars.
Sensitive to touch.
The red rash begins a few days after the pain.
Fluid-filled blisters burst and form scabs.
Itchy, uncomfortable feeling.
High fever.
Headache.
Sensitive to light.
Tired.
Most people with shingles experience pain first. For some, the pain can be severe. Depending on where the pain is, it can sometimes be mistaken for muscle, heart, lung, or kidney problems. Some people also experience pain from shingles without fever or rash.
Is shingles dangerous?
Shingles is usually not dangerous for healthy people, although it can cause pain and burning sensations that make the patient extremely uncomfortable. However, for people with shingles on one side of the face, they must see a dermatologist immediately. Early examination helps limit eye damage, avoid the risk of vision loss or blindness, and avoid shingles scars on the face.
Shingles can lead to pneumonia, hearing problems, blindness, encephalitis or meningitis, and, rarely, death. About 1 in 5 people with shingles will develop severe pain. The pain may continue even after the rash has cleared. This pain is called postherpetic neuralgia (PHN). As you get older, your risk of developing postherpetic neuralgia increases and the disease is more likely to be severe.
Common complications of shingles
1. Postherpetic neuralgia
Your shingles symptoms usually go away when the rash goes away. But with postherpetic neuralgia (PHN), you may feel pain and burning for months or years after the rash has healed. You may experience painful, throbbing episodes that can be uncomfortable and interfere with your daily activities.
This complication is more common in older people (50 years and older). These sensations may disappear after a while or last for many years or may be permanent. Doctors prescribe different medications or therapies to help treat this nerve pain.
2. Itching, tingling (skin sensory disturbance) after shingles
Other sensations associated with postherpetic neuralgia include numbness, tingling, and coldness. Severe cases of postherpetic neuralgia can lead to depression, weight loss, and insomnia.
Postherpetic itching develops in areas of skin that have healed from shingles. Excessive itching and scratching of the shingles scarred skin can lead to skin abrasions, bacterial superinfection, and worsening of the condition.
3. Reduced vision or eye damage
Herpes zoster ophthalmicus (HZO) or shingles occurs near or in the eye, accounting for up to 20% of all cases of shingles. If left untreated, up to 70% of patients with HZO develop serious complications that can include sensitivity to light, swelling of the eyelids, increased eye pressure, inflammation and scarring of the cornea, vision loss, and blindness.
4. Ramsay Hunt syndrome
If you have shingles around your ear, you need to seek treatment as soon as possible. If left untreated, it can lead to Ramsay Hunt syndrome (shingles virus damages the ear, nose and throat organs), causing hearing problems such as earache, hearing loss, and tinnitus.
5. Partial paralysis of facial muscles
Partial facial paralysis is both a symptom of herpes zoster virus infection (facial herpes, also known as trigeminal herpes zoster, trigeminal herpes zoster), and a dangerous complication of herpes zoster.
Usually, the symptoms of hemifacial paralysis or partial paralysis of facial muscles will go hand in hand with skin lesions. You can easily recognize this complication when the face loses expression, the mouth is distorted or the ability to frown or move the muscles on the paralyzed part of the face is lost.
Symptoms of hemifacial paralysis can go away after a while or last forever. Therefore, when hemifacial paralysis occurs, you need to see a doctor for diagnosis and treatment as soon as possible to minimize the danger and complications later.
6. Skin infections
Skin infection or superinfection is a common complication of skin lesions in many patients with shingles. Any lesion on the skin when infected is at risk of superinfection.
In particular, during the blister stage, if the blisters break, it will lead to bacteria and staphylococci entering and causing pus and fluid discharge, worsening skin damage, making the disease worse and easily leaving bad scars.
More dangerously, if not treated early, skin lesions can spread to other areas of the body, leading to blood infection and a very high risk of death.
7. Pneumonia
Pneumonia is a rare but extremely dangerous complication. It mainly occurs in patients with pre-existing immunodeficiency, warning of the risk of death if not treated promptly.
This complication is classified as widespread shingles, a severe level of damage because when diagnosed with widespread shingles, the patient has damage beyond the control of the nerves.
8. Stroke
If the varicella-zoster virus that causes shingles spreads to the brain or spinal cord, serious complications such as stroke and meningitis can occur, especially in people with HZO.
9. Encephalitis
Encephalitis is also a dangerous complication of shingles, which can appear after a few days of skin damage in patients, especially those infected with shingles of the ear. Because the ear has a special structure, connected to the brain system, many dense nerves under the skin, so when the virus appears and penetrates this location, it will increase the risk of spreading the disease to the brain.
Skin lesions inside the ear canal and eardrum area are more dangerous because these are areas that are difficult to care for, clean, and susceptible to secondary infection.
Although dangerous, encephalitis can be completely cured if detected early, intervened promptly and treated properly. However, there are also a few cases of people with encephalitis caused by shingles suffering from severe sequelae such as paralysis, numbness in limbs, epilepsy and even death.
10. Meningitis
Similar to encephalitis, patients with shingles are also at risk of meningitis. When suffering from encephalitis, patients also have a high chance of recovery when receiving good care and treatment. On the other hand, you may also face the risk of dangerous conditions such as paralysis, epilepsy or death if not treated promptly.
When shingles is detected in the ear, patients need to follow the treatment regimen as well as the doctor's instructions to quickly recover and limit dangerous complications.
11. Permanent damage to the nervous system and spine
The shingles virus can cause a number of complications that permanently damage the nervous system and spine. One of the main complications is permanent nerve pain, called postherpetic neuralgia.
12. Danger to the fetus
Shingles during pregnancy rarely causes complications for your baby. If you develop shingles just before or in the days following delivery, protect your newborn from contact with the shingles rash. Covering the rash and washing your hands often are good ways to do this.
13. Death
When shingles spread, the patient has a high risk of death because at this time, the sequelae of shingles may have appeared in the lungs, meninges or severe infections leading to sepsis. In severe cases, if not intervened and treated promptly, the risk of death will be very high.
14. Other rare complications
In a very small number of complications of shingles related to the liver and lungs, causing danger to the central nervous system, especially the brain. When experiencing these complications, patients need to be quickly hospitalized for doctors to diagnose and intervene with immediate treatment.
Prevent complications of shingles
Vaccination against shingles for people at the Vaccination Center, Ho Chi Minh City Dermatology Hospital. (Photo: Dinh Hang/VNA)
1. Vaccination
Vaccination with the recombinant shingles zoster vaccine (Shingrix) is the best way to prevent the disease and its complications.
2. Limit contact with the patient's rashes
Shingles is spread through direct contact with fluid from the rash blisters. The virus can be transmitted to people who have not been vaccinated against shingles and have never had chickenpox.
Even if a person has been vaccinated against shingles, they are still at risk of contracting the shingles virus, but the risk and complications of the disease are lower.
In addition, people with a history of shingles are at high risk of reinfection. You should note that the shingles virus can only be transmitted when the rash blisters appear, but before they appear or after they have crusted over, the possibility of infection is almost zero.
To avoid transmitting the shingles virus to others, patients need to take steps to cover the rash and avoid touching it until it has crusted over. In particular, avoid contact with newborns, children with weak resistance, underweight, pregnant women who have not been vaccinated against shingles or chickenpox, the elderly, and people with weak immune systems./.
(Vietnam+)
Source: https://www.vietnamplus.vn/zona-than-kinh-nhung-bien-chung-nguy-hiem-khong-the-chu-quan-post1037058.vnp

























































































Comment (0)