Today (December 10th), an international conference on epilepsy surgery is being held at Viet Duc Friendship Hospital, bringing together a large number of leading experts from Vietnam and abroad.
Here, experts shared information and exchanged views on many achievements in epilepsy surgery, emphasizing the role of invasive electroencephalography (SEEG) in preoperative assessment.

Vietnam has approximately 710,000 people suffering from epilepsy.
Information presented at the conference revealed that currently, there are approximately 710,000 people with epilepsy in Vietnam, of which about 213,000 are drug-resistant. The annual incidence of epilepsy ranges from 4 to 14 people per 1,000 population. Children with epilepsy account for 30-40% of epilepsy patients in Vietnam.
The number of people with epilepsy in Vietnam compared to other countries such as Japan (870,000), Thailand (50,000), China (nearly 10 million), India (over 10 million)...
Drug-resistant epilepsy (meaning seizures continue despite the use of at least two appropriate anti-epileptic drugs) occurs in approximately 30% of epilepsy patients.
When medication fails to control the condition, surgery is a crucial option for improving quality of life and reducing the risk of long-term complications.
However, one of the key conditions for successful surgery is accurately identifying the epileptogenic zone (EZ): the part of the brain responsible for initiating and propagating epileptic seizures.
If this area is removed or intervened in without significantly damaging normal functions, there is a very high chance that the patient will no longer have seizures or will experience a significant reduction in seizures.
In cases where there is suspicion of complex seizure origin – for example, seizures starting in the deep region, bilateral regions, or unclear magnetic resonance imaging findings – invasive deep electroencephalography (EEG) is necessary. This is where transparenchymal EEG (SEEG) becomes very valuable.
What is transparenchymal electroencephalography (EEG)?
Information presented at the conference indicated that Stereo-Electroencephalography (SEEG) is a technique that involves placing depth electrodes through the skull into the brain, precisely positioning them in three dimensions, to record brain electrical activity from deep and complex regions.
Thanks to this approach, doctors can collect electroencephalogram (EEG) data during extra-operative monitoring in multiple regions simultaneously – compared to more superficial methods such as surface electrode grids.
Transparenchymal electroencephalography (EEG) offers significant advantages, such as access to deep brain regions like the hippocampus, amygdala, insular lobes, and medial/central hemispheres—areas often difficult to access with surface electrodes; and it is less invasive than craniotomy for subdural electrode placement (SDE).
This also allows for more precise identification of the epileptic seizure initiation and propagation network, thereby increasing the chances of surgical success.
One of the major concerns is "is deep electrode placement safe?" According to information presented at the conference, current studies show that the complication rate of this method is low. For example, in a systematic analysis of 57 articles and over 2,500 patients: the bleeding rate was approximately 1% and the infection rate was approximately 0.8%. The overall complication rate was approximately 1.3%.
In terms of overall safety: transparenchymal electroencephalography (EEG) is considered "safe and effective" when performed in a large surgical center with good procedural standards.
However, neurosurgeons also emphasize that any invasive procedure carries risks—bleeding in the brain, damage to small blood vessels, electrode site infection, or complications after cutting/surgery. Therefore, doctors must always carefully weigh the potential benefits against the risks, and patients need thorough counseling before undergoing the procedure.
Epilepsy surgery: A life-saving solution for patients with drug-resistant epilepsy.
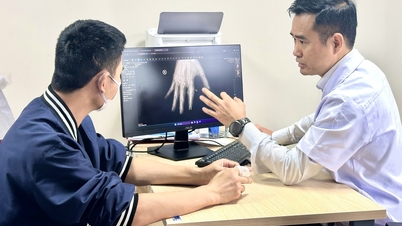
Associate Professor Dr. Dong Van He - Deputy Director of Viet Duc Friendship Hospital and President of the Vietnam Neurological Association - said that over the past 10 years, the hospital's Neurosurgery Center has examined and screened hundreds of thousands of epilepsy patients, including many complex cases.
Doctors here have also performed surgery on over 150 cases of drug-resistant epilepsy, using important and modern diagnostic systems such as a 3.0 Tesla MRI machine, applying the internationally standardized HARNESS protocol, PET CT, and video electroencephalogram (EEG) system.
"The results show that seizure control reaches up to 80%, bringing about a significant improvement in the quality of life for patients," said Associate Professor Dr. Dong Van He.
The expert also emphasized that epilepsy surgery is increasingly becoming a lifesaver for patients with drug-resistant epilepsy, and that accurately identifying the seizure site is a crucial factor in its success.
The trend of adopting SEEG is increasing globally, especially in specialized centers in the US, Europe, China, and India.
"In Vietnam, with the development of neurosurgery and neuroelectrophysiology, SEEG is an important direction for improving the effectiveness of epilepsy surgery, helping many patients overcome seizures and improve their quality of life," said Assoc. Prof. Dr. Dong Van He.
Source: https://suckhoedoisong.vn/ky-thuat-mo-moi-giup-hang-tram-nghin-nguoi-bi-dong-kinh-khang-thuoc-nang-chat-luong-song-169251210153650029.htm







































![[Video] The craft of making Dong Ho folk paintings has been inscribed by UNESCO on the List of Crafts in Need of Urgent Safeguarding.](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/12/10/1765350246533_tranh-dong-ho-734-jpg.webp)



































































Comment (0)