In Ho Chi Minh City, Mr. Tuan, 43 years old, snored due to tonsillitis, hypertrophic turbinates, and pharyngeal stenosis. He underwent endoscopic surgery to correct the inferior turbinate and soft palate, and to remove his tonsils.
The results of Mr. Tuan's ENT endoscopy at Tam Anh General Hospital in Ho Chi Minh City showed hypertrophic tonsillitis (recurrent tonsillitis causing swelling), hypertrophic inferior turbinate on both sides, and pharyngeal isthmus narrowing. The pharyngeal isthmus is the posterior part of the throat including the soft palate, uvula, tonsils, and base of the tongue.
On December 4th, Dr. Pham Thai Duy, a specialist in Otolaryngology at the Ear, Nose, and Throat Center, stated that several factors contribute to nasal congestion and "thunderous" snoring in patients. An enlarged turbinates obstruct nasal breathing, especially during sleep. A narrowed pharynx increases pressure on the airway, leading to long-term pharyngeal edema, causing nasopharyngitis, hypertrophic tonsillitis, and snoring.
Considering the advantages and disadvantages of medical and surgical treatments, the doctor advised a "3-in-1" surgery for the patient, including endoscopic inferior turbinate reshaping, tonsillectomy, and uvula and soft palate reshaping. Uvula and soft palate reshaping surgery helps to widen the airway in the pharyngeal region by removing soft tissue from the soft palate and lateral pharyngeal walls, possibly with tonsillectomy.
According to Dr. Tran Thi Thuy Hang, Head of the Ear, Nose, and Throat Department, the "3-in-1" surgery helps reduce the number of procedures, but patients will have two incisions in their mouth and nose, which can cause more discomfort. To overcome this, the team successively removed the tonsils and reshaped the soft palate and uvula using Coblator technology, which helps to cut, cauterize, and control bleeding at the site, minimizing damage to healthy tissue. Afterward, a partial inferior turbinate resection was performed endoscopically, reducing the risk of infection and preserving nasal and sinus function.

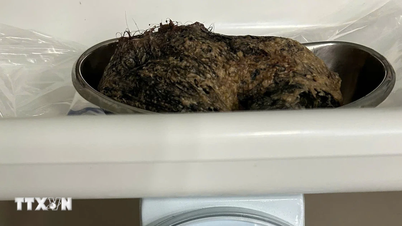
Doctor Thai Duy (right) and his team perform laparoscopic surgery on a patient. Photo: Tam Anh Hospital
Mr. Tuan was discharged from the hospital two days after surgery. His health is stable; he can talk, has no discomfort in his nose and throat, sleeps better, and has stopped snoring.
Dr. Hang further explained that pharyngeal stenosis has varying degrees of severity. In severe cases, snoring not only affects those around the snorer but also exacerbates existing medical conditions such as hypertension and diabetes, increasing the risk of stroke. This is also a cause of sleep apnea syndrome.
Treating snoring requires the collaboration of multiple specialties, including Otolaryngology, Respiratory Medicine, Neurology, etc. Complex cases require interdisciplinary consultations and imaging and functional tests such as ENT endoscopy, spirometry, polysomnography, and maxillofacial CT scans to determine the cause and appropriate treatment.
Patients are advised on non-invasive (using ventilators) and invasive treatment methods (including surgery to treat nasal congestion, nasopharyngeal and uvula corrective surgery, jaw surgery, and radiofrequency ablation). Generally, a combination of methods yields better results.
According to Dr. Hang, regardless of the treatment method chosen, the ultimate goal is for patients to improve their sleep, eliminate snoring, and have their underlying medical conditions better controlled.
After surgery, patients need to maintain a healthy lifestyle, exercise, eat a healthy diet, and effectively manage nasal and sinus conditions to prevent recurrence.
Khanh Ngoc
* Patient's name has been changed
| Readers can ask questions about ear, nose, and throat diseases here for doctors to answer. |
Source link
















































































































Comment (0)