Medical news update September 5th: Why are so many people getting flesh-eating bacteria?
According to Hoa Binh Provincial General Hospital, they are currently treating two patients with Whitmore's disease (an infection caused by "flesh-eating" bacteria). One of the patients has a serious prognosis and is receiving intensive treatment and care.
More cases of flesh-eating bacteria have been reported.
Accordingly, the first patient is Ha Ngoc T. (43 years old, residing in Da Bac district, Hoa Binh province), who has been working as a factory worker in a southern province for over 10 years, his daily job being delivering frozen goods to distributors.
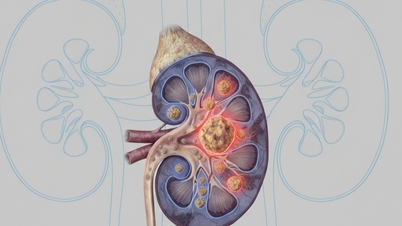
 |
| Illustrative image |
Prior to hospitalization, patient T. had been discharged with a persistent high fever. Despite medical examinations and treatment, the fever only subsided, not completely disappeared. On August 28th, the family requested that the patient be discharged from treatment and return to their hometown (Hoa Binh province).
Upon arriving in Hoa Binh, the patient was admitted to the hospital in a critical condition with high fever, chills, respiratory failure, septic shock, and multiple organ failure. The patient was quickly placed on a ventilator, underwent continuous hemodialysis, received vasopressors, and was given broad-spectrum antibiotics, including antibiotics specifically for Whitmore's disease.
Clinical findings revealed that the patient had bilateral pleural effusion and effusion, and a septic liver abscess caused by the bacterium Whitmore's disease (Burkholderia pseudomalle).
Currently, patient T. remains in critical condition, receiving intensive treatment and care, and undergoing consultations with multiple specialists.
The second patient is Bui Thi C. (59 years old, from Lac Son, Hoa Binh), with a history of diabetes. Before being admitted to the hospital, the patient had a high fever, swelling, heat, redness, pain in the right wrist, cough and increasing difficulty breathing.
Patient C. was admitted with respiratory failure requiring non-invasive mechanical ventilation, persistent high fever, chills, signs of infection and toxicity, productive cough, an abscess in the right wrist, and a CT scan showing consolidation and bilateral pleural effusion.
Patient C. is now out of critical condition. She is expected to be discharged in about a week and will continue maintenance treatment with oral medication at home for 3 to 6 months.
Whitmore disease is not a new disease in Vietnam. Every year, the whole country has about 100-200 people suffering from this disease. Since the beginning of the year, Tam Anh General Hospital in Ho Chi Minh City has treated more than 10 cases, including 4 cases that occurred in the last 3 months, which is the rainy season in the Southern region.
The flesh-eating bacteria Burkholderia pseudomallei that causes Whitmore disease is a gram-negative bacterium that can survive in harsh conditions such as nutrient-poor, dry environments. They often live in naturally moist soil environments, especially the soil layer 20-40 cm below the surface.
This bacteria has the ability to cause strong inflammation, leading to damage to surrounding tissues and structures, including the discs and vertebrae.
The main route of infection is through damaged skin coming into direct contact with contaminated soil or through inhalation of contaminated soil particles.
The disease often occurs in people who are frequently in contact with soil and water such as farmers, construction workers, gardeners, soldiers, etc.
Whitmore disease can occur in humans and animals such as dogs, cats, cows, horses, mice and is often scattered throughout the year but increases during the rainy season.
This disease occurs at all ages, with men generally having a higher incidence rate than women. Individuals with underlying conditions such as diabetes, alcoholism, long-term corticosteroid use, chronic lung and kidney disease, etc., are at a higher risk of infection compared to the general population.
The disease can also occur in people who were previously completely healthy and there have been no recorded cases of transmission between humans and animals.
Recent environmental investigations have shown that over 80.0% of soil samples in southern Vietnam tested positive for Burkholderia pseudomallei bacteria. People should use protective equipment (such as boots and gloves) and bandage open wounds, cuts, or burns if they have close contact with soil or water.
People at high risk should avoid going outside after heavy rain, especially in rural areas, to prevent the risk of Whitmore disease.
Since there is no vaccine to prevent the disease, people need to wash their hands frequently before and after preparing food, before eating, after using the toilet, and after working in the fields.
Do not bathe, swim, or dive in ponds, lakes, or rivers in or near contaminated areas. If you have open wounds, ulcers, or burns, avoid contact with potentially contaminated soil or water.
When patients have symptoms of prolonged high fever, skin and soft tissue infections, pneumonia, abdominal pain, back pain, headache, etc., they should go to medical facilities with high technical expertise for early diagnosis and treatment.
New information on the case of many students hospitalized in Thai Nguyen.
The People's Committee of Thai Nguyen province directed the Department of Health to collect samples and send them to the Central Hospital for Tropical Diseases for testing to clarify the cause of the incident.
According to information from the People's Committee of Thai Nguyen province, no new cases related to the mass hospitalization of students from Thai Nguyen Industrial College have been recorded in the province. The health condition of the patients under treatment is progressing well and is basically stable.
Tests conducted at medical facilities throughout the province have so far determined the cause of the recent wave of unusual hospitalizations among students.
The People's Committee of Thai Nguyen province has instructed the Department of Health to collect samples and send them to the Central Hospital for Tropical Diseases for analysis and testing to determine the cause.
It is known that after the incident, the Steering Committee for Disease Prevention and Control of Thai Nguyen province issued a document requesting heads of departments, branches and sectors to strengthen close direction of disease prevention and control work in the province.
Continue to strictly implement the directives of the Ministry of Health and the People's Committee of Thai Nguyen province in proactively deploying disease prevention and control measures during the back-to-school season.
The Department of Health, Thai Nguyen Central Hospital, and the Thai Nguyen Provincial Center for Disease Control (CDC) are closely monitoring cases to prevent the spread of the disease in the community.
Working closely with the National Institute of Hygiene and Epidemiology to assess risks, analyze the situation, and develop effective response plans for potential disease outbreaks.
Provide effective guidance on patient admission and treatment, infection control, and prevention of cross-infection in healthcare facilities...
All students in the three dormitory rooms where patients died or were hospitalized have been isolated, and daily meals are being provided in their rooms.
Clean floors, doorknobs, stairs, etc., with a regular disinfectant solution.
The school's 1,102 students, including 486 boarding students and 212 students from Ha Giang, were notified to monitor their health and inform the school if they experience any unusual symptoms.
The Thai Nguyen City Health Center continues to closely monitor and supervise the school, guiding the implementation of isolation, disinfection, and environmental hygiene measures.
Fully implement the infectious disease reporting and information system as stipulated in the Ministry of Health's circular on guiding the reporting and declaration of infectious disease outbreaks.
Previously, on September 2nd and 3rd, a number of students from Thai Nguyen Industrial College were hospitalized with unusual symptoms, and one case resulted in death.
Immediately after receiving information about the incident, the People's Committee of Thai Nguyen province directed the inspection and resolution of the matter. The Department of Medical Examination and Treatment Management, Ministry of Health, also requested medical facilities to support Thai Nguyen in treating the patients.
How can we prevent kidney stones?
If kidney stones are left untreated for a long time, they can lead to several dangerous complications such as hydronephrosis, urinary tract infection, nephritis, kidney abscess, renal parenchymal atrophy, impaired kidney function, and even bloodstream infection, which can threaten the patient's life.
In 70-80% of cases of kidney stones, the patient can pass the stones out of the body through the urinary tract. However, the case of passing stones during normal urination only occurs with small kidney stones.
According to Assoc. Prof. Dr. Vu Le Chuyen, Director of the Urology and Nephrology Center at Tam Anh General Hospital in Ho Chi Minh City, the larger the kidney stone, the greater the risk of it becoming lodged.
Normally, a stone with a diameter smaller than ≤ 5mm is likely to pass out naturally, and only larger stones, with a diameter greater than > 5mm, can become lodged.
Two factors influence the likelihood and rate of spontaneous elimination of kidney stones: the size and location of the kidney stones.
The size of kidney stones is a key factor in determining whether they can be naturally passed. 80% of these stones are smaller than 20%.
Patients only need treatment for kidney stones measuring 4-6mm. However, about 60% of kidney stones of this size are still passed naturally. This process takes an average of 45 days.
Larger stones (> 6mm) usually require medical treatment to remove them from the body. Only about 20% of stones of this size can be passed naturally. However, the process often takes a long time, up to a year.
Stones located at the end of the ureter, near the bladder (not at the end where it attaches to the kidney), are more likely to move and be expelled from the body during normal urination.
Studies show that about 79% of these stones will pass away on their own. 48% of stones located in the lower part of the ureter near the bladder will pass out of the body during urination without any medical treatment.
Patients should drink plenty of water and exercise regularly. Jumping rope is a very good option. This can help loosen stones and increase the chances of their natural expulsion, especially lower renal calyx stones.
When kidney stones are newly formed and have not caused complications, and the urinary tract is wide and free from congenital deformities or narrowing, the body may pass stones measuring 2-3 mm, or even up to 8-9 mm. Doctors can help patients urinate more easily by advising them to drink plenty of water and take anti-inflammatory medication to prevent edema in the urinary tract lining that could obstruct the stones.
Additionally, doctors may prescribe medications to dilate the urinary tract, making it easier to expel kidney stones from the body. Therefore, not all kidney stones require surgery. Many cases can be treated with medication.
An adult's kidney is approximately 12cm long. Therefore, if kidney stones are smaller than 5mm, patients only need to take medication and drink plenty of water. The stones can be naturally passed through the urinary tract. Kidney stones measuring 5-7mm are not a major problem; concern only arises when kidney stones cause infection or recur frequently.
Kidney stones can cause infections. However, infections can also cause kidney stones. Therefore, when a kidney stone patient experiences symptoms of a urinary tract infection, both the kidney stones and the urinary tract infection need to be treated simultaneously. This will help to completely resolve the condition.
During treatment, patients may be prescribed medication or subcutaneous lithotripsy. However, the infection must be completely treated first. If the infection persists, the doctor cannot proceed with lithotripsy surgery. Furthermore, if the infection recurs, the risk of stone formation after lithotripsy is high.
For large kidney stones, open surgery is the appropriate treatment method, allowing for complete removal of the stone. Open surgery was previously the optimal, neatest, and most cost-effective method.
Open surgery has the advantage of completely removing the stones. However, nowadays there are many advanced surgical methods to gradually break down the stones and remove them from the body.
If the kidney stone is small (only 1cm), and is radiopaque, not too hard, the doctor can apply the method of extracorporeal lithotripsy. The advantage of this method is that it is less invasive, does not require hospitalization and is quite cheap. Sometimes, kidney stones can not be completely crushed in one session. The patient may need to perform lithotripsy 2-3 times to completely destroy them.
When kidney stones have moved down the ureter near the bladder, doctors may use a semi-rigid endoscope and laser lithotripsy. If the kidney stones are still located higher up, doctors will use a flexible endoscope to remove them.
When kidney stones are located in the mesonephros, doctors will use a percutaneous nephrolithotomy device to make a small hole in the kidney to break up the stones. This endoscopic lithotripsy method is most commonly used at Tam Anh General Hospital due to its minimally invasive advantages. Patients experience no pain, minimal bleeding, and a faster recovery. Furthermore, high-resolution 2D-3D screens help doctors accurately and completely remove the stones from the kidney.
In addition, doctors advise everyone to have regular health checkups every 6-12 months to detect kidney stones in particular, and urinary tract stones in general, early so that appropriate treatment can be implemented.



![[Photo] Closing Ceremony of the 10th Session of the 15th National Assembly](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F11%2F1765448959967_image-1437-jpg.webp&w=3840&q=75)



![[Photo] Prime Minister Pham Minh Chinh holds a phone call with the CEO of Russia's Rosatom Corporation.](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F11%2F1765464552365_dsc-5295-jpg.webp&w=3840&q=75)












































![[OFFICIAL] MISA GROUP ANNOUNCES ITS PIONEERING BRAND POSITIONING IN BUILDING AGENTIC AI FOR BUSINESSES, HOUSEHOLDS, AND THE GOVERNMENT](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/12/11/1765444754256_agentic-ai_postfb-scaled.png)


















































Comment (0)