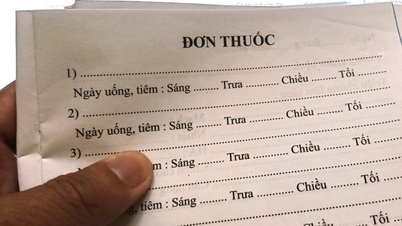
The Ministry of Health has just issued Circular No. 01/2025/TT-BYT detailing and guiding the implementation of some articles of the Health Insurance Law. This includes a list of 62 rare and critical illnesses that do not require a referral letter, allowing patients to still receive 100% health insurance coverage (as stipulated in point a, clause 4, Article 22 of the Health Insurance Law) when seeking medical treatment at specialized facilities.
According to the Ministry of Health , individuals covered by health insurance who fall under the categories specified in this list are not required to transfer to another medical facility. The list most frequently includes malignant tumors, metabolic disorders, and congenital defects.

Specifically, the following diseases are eligible for benefits immediately upon receiving a confirmed diagnosis: tuberculous meningitis (G01*); tuberculous meningioma (G07*); other types of nervous system tuberculosis; unspecified nervous system tuberculosis (G99.8*); pulmonary mycobacteria infection; acute pulmonary histoplasma capsulatum infection; acute pulmonary blastomyces infection; pulmonary paracoccidioides infection; pulmonary sporotrichum infection (J99.8*); invasive pulmonary aspergillus infection; pulmonary cryptococcus infection; pulmonary mucor infection; disseminated mucor infection…
Heart failure patients who have been diagnosed with stage 3 or stage 4 are immediately referred to specialized care.
Patients with malignant tumors (coded from C00 to C97) who meet the following criteria will be directly admitted to specialized care without going through the prescribed referral procedure (also known as bypassing the referral system): those under 18 years of age; this does not apply to cases with a confirmed diagnosis but without a specific treatment indication.
For patients with diabetes, certain conditions must be met to be directly admitted to the intensive care unit. For example, insulin-dependent patients (code E10.7) with grade 2 foot ulcers or stage 3 or higher chronic kidney disease, or at least two of the following complications: cardiovascular, ocular, neurological, or vascular. Non-insulin-dependent patients (code E11.7) with grade 2 foot ulcers or stage 3 or higher chronic kidney disease.
Individuals participating in health insurance are entitled to benefits after being diagnosed with a disease included in the list of 62 diseases and disease groups in Circular 01/2025/TT-BYT.
If the patient's condition has stabilized after treatment, or as required by medical professionals, the healthcare facility may transfer the patient back to a primary or basic healthcare facility for continued monitoring and treatment.
According to the current Law on Medical Examination and Treatment, the medical examination and treatment system is divided into 3 professional levels: initial - basic - advanced (instead of 4 levels: central - provincial - district - commune).
Prior to 2024, individuals suffering from certain serious illnesses, severe diseases, or diseases requiring advanced medical techniques who wished to be treated at a higher-level facility (not their initial health insurance registration location) had to follow a procedure of obtaining a referral letter within the year from a lower-level medical facility to a higher-level facility with sufficient treatment capacity.
A representative from the Health Insurance Department of the Ministry of Health stated that the list of diseases that can be referred to higher-level facilities without a referral letter "are diseases that can only be treated at higher-level facilities," and has been carefully studied to ensure that there is no overload at the final-level facilities.
The Ministry of Health assesses that eliminating this referral procedure will help streamline procedures, create convenience, reduce costs for people, and save money for the Health Insurance Fund.
Source: https://kinhtedothi.vn/62-benh-hiem-hiem-ngheo-khong-can-giay-chuyen-tuyen-van-duoc-huong-100-bhyt.html





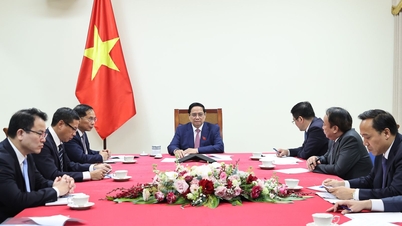
![[Photo] Prime Minister Pham Minh Chinh holds a phone call with the CEO of Russia's Rosatom Corporation.](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F11%2F1765464552365_dsc-5295-jpg.webp&w=3840&q=75)
![[Photo] Closing Ceremony of the 10th Session of the 15th National Assembly](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F11%2F1765448959967_image-1437-jpg.webp&w=3840&q=75)



















































![[OFFICIAL] MISA GROUP ANNOUNCES ITS PIONEERING BRAND POSITIONING IN BUILDING AGENTIC AI FOR BUSINESSES, HOUSEHOLDS, AND THE GOVERNMENT](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/12/11/1765444754256_agentic-ai_postfb-scaled.png)





















































Comment (0)