Thyroid cancer is becoming increasingly common, especially in women. Thyroid nodules detected by neck ultrasound are no longer rare, but amidst conflicting information, many people either become too frightened and rush to have surgery, or they carelessly ignore signs of malignancy.
In the online seminar "Thyroid Surgery: What Doctors Want You to Understand Correctly" organized by Dan Tri newspaper, MSc. Dr. Nguyen Xuan Quang, Head of the Department of Otolaryngology and Head and Neck Surgery, Hong Ngoc Phuc Truong Minh General Hospital, shared key information to help patients be aware of their illness.
Human papillomavirus infection is very common, so don't panic and don't underestimate it.
According to Dr. Nguyen Xuan Quang, the appearance of an abnormal nodule or mass in the thyroid gland is extremely common.
It is estimated that 60 to 70, or even 80% of the population will have at least one thyroid nodule detected during an ultrasound examination, especially in women. This news may be shocking, but the good news is that most of these nodules are benign and do not require any intervention, only regular monitoring.
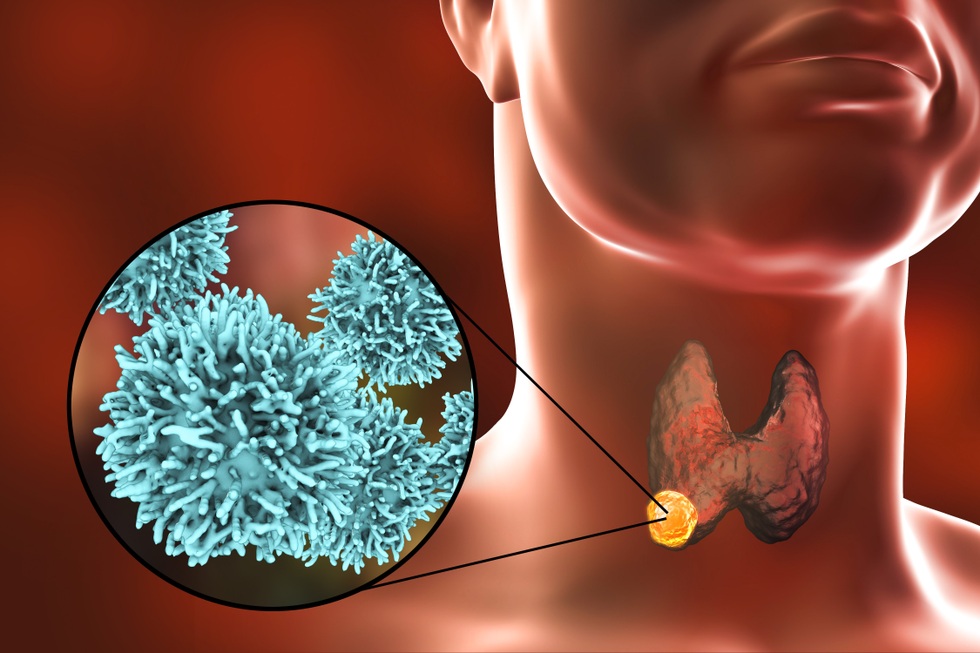
It is estimated that 60 to 70, or even 80% of the population will have at least one thyroid nodule detected during an ultrasound examination, especially in women (Photo: Getty).
According to the doctor, the crucial point is the patient's attitude upon receiving the ultrasound results showing a thyroid nodule. Dr. Quang emphasized that both extremes are dangerous. One is excessive panic, immediately seeking a biopsy and demanding surgery upon hearing about a nodule. The other is complacency, reading somewhere that "thyroid cancer is not dangerous" and then ignoring it, failing to get re-examined or monitored.
"First, there's no need to panic or worry, but we shouldn't be complacent either. Patients need to go to reputable facilities and see experienced doctors for thorough assessment and proper advice, avoiding two equally dangerous situations: overtreatment or missing the golden opportunity for treatment," said Dr. Quang.
The biggest question when a thyroid nodule is detected is, "Is it something to worry about?" According to Dr. Quang, current medical science relies on two main pillars to assess the risk of malignancy before surgery: ultrasound and fine-needle aspiration cytology.
On ultrasound, doctors use the TIRADS classification system with 5 levels. TIRADS 1, 2, and 3 are usually benign and only require monitoring. TIRADS 4 and 5 are the group with more suspicious factors for cancer; depending on the size, the doctor will order a fine-needle aspiration biopsy.
Fine-needle aspiration biopsy, or cell fine-needle biopsy, involves inserting a very small needle into a tumor and extracting a small sample of cells for microscopic examination.
Because a tumor can contain many different types of cells, the results are divided into 6 groups, from group 1 (insufficient cells to draw a conclusion), group 2 (benign), to group 6 (typically cancerous).

Dr. Nguyen Xuan Quang, Head of the Department of Otolaryngology and Head and Neck Surgery, Hong Ngoc Phuc Truong Minh General Hospital (Photo: Hai Long).
Groups 3 and 4 are "intermediate" groups, with atypical or cystic cells, and a cancer risk of approximately 30 to 40% and even higher, respectively. Group 5 is concluded to be suspected cancerous.
Dr. Quang noted that these groups only reflect the clarity of the conclusion, not the "malignancy" of the tumor.
More importantly, while combining ultrasound and fine-needle aspiration cytology can differentiate between benign and malignant with over 95 percent accuracy, no method is absolutely foolproof. There are still cases where a poor ultrasound result suggests malignancy, but the needle lands on a healthy area, resulting in a provisional benign diagnosis.
"If a biopsy reveals cancer, it's almost certainly cancer. If it reveals a benign lesion, it's not necessarily a complete cure. Many factors need to be considered to provide the most accurate advice to the patient," Dr. Quang emphasized.
When is surgery necessary, and when is monitoring sufficient?
Not all thyroid nodules require surgery. Dr. Quang clarified:
The first group consists of malignant or suspected malignant tumors. The majority of these cases will require intervention, primarily surgery, although there are some exceptional cases that are closely monitored rather than immediately operated on.

According to Dr. Quang, not every thyroid nodule requires surgery (Photo: Hai Long).
The second group consists of benign tumors that are large enough to deform the neck or cause compression leading to difficulty swallowing, breathing problems, or hoarseness. In these cases, even though benign, the tumor still affects function and aesthetics, making surgery a reasonable option.
The remaining small, benign tumors, usually under 2cm, do not cause discomfort, and doctors believe they can be monitored periodically every one to two years without intervention. This also helps avoid unnecessary surgery on a very important endocrine organ.
Notably, with regard to thyroid cancer itself, current treatment protocols worldwide have incorporated the concept of "active monitoring" for very small tumors, under 5mm or 1cm, that are differentiated, low-risk, confined within the thyroid gland, and not close to the capsule or vital structures.
These cases are allowed to postpone surgery, with close monitoring via ultrasound every 6 months or 1 year. Surgery is only performed if the tumor grows rapidly in size, exceeds safe limits, or if abnormal lymph nodes appear.

One of the questions Dr. Quang receives almost daily is, "Will I have my entire thyroid gland removed or just a part of it?" (Photo: Hai Long).
"This is cancer, but there may still be no immediate action needed. Many patients are monitored for 5 to 10 years and the tumor doesn't progress to a dangerous level," the doctor said, emphasizing that this decision must be carefully considered and individualized for each person, and is more suitable for older people with very early-stage disease.
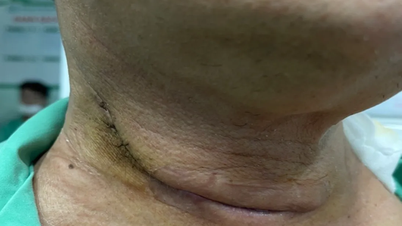
Endoscopic thyroidectomy: When can it be performed?
One of the questions Dr. Quang receives almost daily is, "Will I have my entire thyroid gland removed or just a part of it?"
Previously, when discussing thyroid cancer, the general principle was to completely remove the thyroid gland to ensure "radical eradication," after which the patient would take hormone replacement therapy for life.
In recent years, many large studies have shown that with early-stage, low- or moderate-risk thyroid cancer, doctors can completely remove only the thyroid lobe containing the tumor, leaving the other lobe intact, and still control the disease well.
The decision on how much tissue to remove depends on many factors. Besides age, gender, family history, and comorbidities, the most important are the characteristics of the tumor: size, location, degree of invasion, presence of suspected lymph nodes with metastasis, and the number and location of lymph nodes. Based on these factors, the doctor classifies the patient into a low, medium, or high risk group for recurrence.

Modern techniques provide excellent support for thyroid cancer surgery (Hong Ngoc).
Recently, endoscopic thyroidectomy via the oral vestibule has attracted much attention, especially from women, because it leaves no external scars. The instrument is inserted through the mucous membrane of the lower lip, a short distance to the thyroid gland, with minimal impact on healthy tissue, and can access both thyroid lobes from a single entry point.
However, Dr. Quang emphasized that this is not a "method for everyone." Endoscopy through the mouth is only applied to very early-stage cancers, where the tumor is usually less than 2cm, located within the thyroid gland, and the thyroid gland is not too large. Some large centers may have slightly broader indications, but the general principle remains to select small, early-stage tumors.
"For tumors that are suitable for treatment, laparoscopic surgery can completely resolve the problem and effectively control the central lymph node system. However, the most important factor remains the stage of the disease and the correct choice of treatment. We cannot sacrifice the thoroughness of cancer treatment for aesthetic reasons," said Dr. Quang.
At Hong Ngoc Phuc Truong Minh General Hospital, a key advantage is its team of surgeons with extensive experience in the field of head and neck oncology.
Dr. Quang stated that he has personally performed thousands of thyroid surgeries over the past nearly 15 years, including new techniques such as endoscopy and surgery through the vestibular-oral approach to minimize scarring in the neck area.

At Hong Ngoc Phuc Truong Minh General Hospital, a key advantage is the surgical team's extensive experience in the field of head and neck oncology (Photo: Hai Long).
Experience has enabled the team not only to master surgical procedures but also to gain a thorough understanding of potential misjudgments in thyroid nodule assessment. This allows them to guide patients on when surgery is necessary and when monitoring is sufficient, thus avoiding excessive intervention.
Modern technology reduces complications.
Among the complications of thyroid surgery, damage to the recurrent laryngeal nerve is considered the most concerning, as this nerve controls the voice.
If the vocal cords are damaged, the patient may experience hoarseness or loss of voice, temporarily for a few weeks or permanently. In more severe cases, damage to both vocal cords can cause them to close, making it impossible for the patient to breathe, requiring a tracheostomy to ensure an open airway.

Among the complications of thyroid surgery, damage to the recurrent laryngeal nerve is considered the most concerning, as this nerve controls the voice.
In addition, hypocalcemia can be a complication affecting the parathyroid glands, which are very small endocrine glands located close to the thyroid gland but play a role in maintaining calcium levels.
To minimize these complications, at Hong Ngoc Phuc Truong Minh General Hospital, Dr. Quang said that the surgical team applies modern supporting technologies such as the Neuroimaging Device (NIM).
This is a state-of-the-art device that assists in identifying, monitoring, and maximally protecting the laryngeal nerve that controls voice during surgery, along with a specialized lighting system to detect parathyroid glands. These technologies are not available at all facilities, and when applied correctly, they significantly reduce risks, especially in complex or revision surgeries.
After surgery, do I have to take medication for life and follow a strict diet?
The thyroid gland is an essential hormone-secreting organ for the body. When the entire thyroid gland is removed, the patient is required to take hormone replacement therapy for life.
If only a partial thyroidectomy is performed, some cases may still result in the remaining thyroid gland producing enough hormones, but others may require supplementation to compensate for the deficiency and reduce the risk of recurrence. The dosage will be adjusted periodically by an endocrinologist; there is no single formula that applies to everyone.

According to Dr. Quang, patients need to understand their condition and follow their doctor's instructions to achieve the best results (Photo: Hai Long).
Regarding diet, in cases where only a portion of the thyroid gland has been removed and radioactive iodine treatment is not administered, patients are encouraged to supplement their diet with iodine-rich foods such as eggs, milk, seafood, and dark green vegetables to help the remaining thyroid gland function properly.
Conversely, for individuals preparing for radioactive iodine treatment after total thyroidectomy, from post-surgery until before taking the radioactive iodine, the body needs to be "iodine deficient," so they must almost completely avoid all sources of iodine, including iodized salt, seafood, and some dairy products.
Regarding follow-up appointments, in the first year after surgery, patients are usually scheduled for check-ups every 3 to 6 months, with the 3 to 4 weeks post-surgery mark being particularly important for checking thyroid function and adjusting medication. In the second year, the interval between check-ups is approximately 6 months. From the third year onwards, most patients only need a check-up once a year, unless there are any abnormalities.
Source: https://dantri.com.vn/suc-khoe/phat-hien-khoi-uo-tuyen-giap-khi-nao-can-phai-mo-20251211082429626.htm


















































































































Comment (0)